Using an A15 automatic biochemical analyzer will give you a number of advantages over the use of a semi-automatic:
There are major differences when it comes to the quality that LEDs offer. HEINE has set a new standard which maintains that only the best is good enough, from the selection of materials to processing, from light intensity to dimmability, and from thermal management to a colour rendering index as high as possible.That’s what we call LED in HEINE Quality – or LED HQ.
See the difference for yourself when using a HEINE LED instrument. See the colours as they are during each examination.

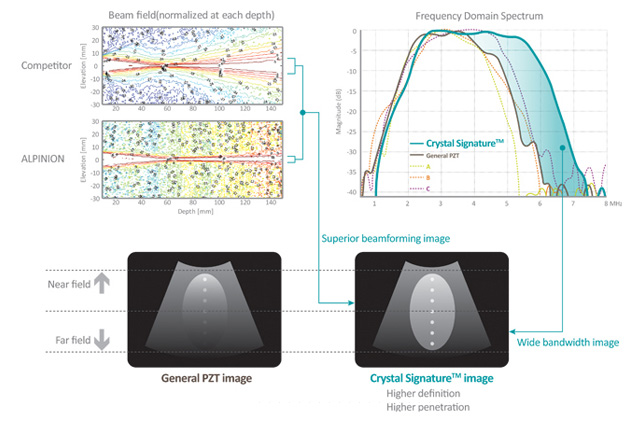
A transducer converts a signal in one form of energy to another form of energy. A transducer transmits and receives reflected ultrasound signals that are the primary data source for the creation of ultrasound images. Proprietary transducer technology yields superior clinical ultrasound imaging.

ALPINION’s transducer portfolio includes conventional piezo-ceramic,composite PZT and the latest single crystal materials. Single crystal material produces broadband frequency response and higher sensitivity, permitting its use in harmonic imaging with minimal loss of the acoustic signal. It results in more uniform wide-bandwidth imaging and thus offers higher resolution images to the user.
ALPINION has overcome the historic engineering and application limitations in the processing of delicate and expensive single crystal transducer materials through a unique and proprietary fabrication process. With ALPINION’s high performance single crystal transducer, users acquire broadband images with unparalleled sensitivity.
Through a unique and innovative single crystal transducer processing technology, ALPINION has produced the largest single crystal convex transducer ever fabricated, and the world’s first 3D/4D transducer made with single crystal material.
A single crystal transducer is characterized by a higher energy conversion efficiency and higher sensitivity than conventional piezo-ceramic materials; consequently, single crystal transducers can produce greater uniformity, and stronger penetration.
The attention to ergonomic design extends to the flexible cable and lightweight handle that are standard on all ALPINION transducer products.
Driven by customer requirements, ALPINION has accomplished the following:
• Ergonomic Transducer design with a flexible cable supports pain-free wrist manipulation when imaging.
• LabelingFluorescent labels on the transducer enable users to identity the transducer ID easily under subdued lighting conditions.
• 3D/4D transducersLightweight 3D/4D transducers with improved detail accuracy by overcoming size limitation and manufacturing difficulties.
Crystal Signature™ is characterized by much higher energy conversion efficiency than conventional piezo-ceramic materials, yielding greater uniformity and sensitivity. When combined with unique manufacturing processes, our proprietary Crystal Signature™ technology gives better images while decreasing production costs.
MicroFit™ Technology has resulted in smaller and lightweight transducers with better ergonomics that reduce operator fatigue.
Special attention is paid to the transducer cable, which is the lightest and most flexible in the ultrasound industry, further reducing the strain on the operator. Image quality is preserved under all conditions with the tough and robust connectors, which utilize the latest micro-pinless interconnect technology.
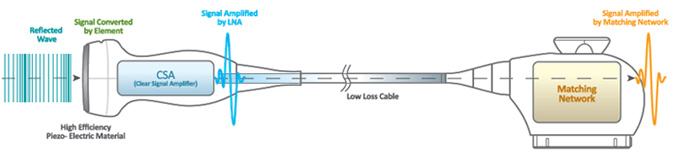
SensitiView™ Technology
The CSA™ generates an enriched purified signal with active electronics from high quality piezo-electric materials.

Endoscopic ear surgery is the latest technique for performing surgical interventions on the hearing organs and is being actively introduced throughout the world. In some cases, endoscopic ear surgery may result in a less invasive operation that can be performed entirely through the ear canal. The endoscope is one of two tools surgeons can use to see well during ear surgery. The other tool is a specialized microscope.
Microscopes have been used in otology for over seventy years. They make structures appear larger and have a very bright light. Surgical microscopes are large devices, weighing hundreds of pounds. The lens of the microscope needs to be about a foot away from the object (or target) the surgeon is looking at. As a result, other structures between the target and the lens can block the view. To overcome blocked views, surgeons sometimes need to make a larger incision (for example behind the ear canal) or drill away bone.
An endoscope is another type of device that can help surgeons see during surgery. It is shaped like a narrow tube and the lens is at the tip. The lens can be placed extremely close to the target, less than half an inch (or thirty times closer than with the microscope). This allows a very detailed view. Because the endoscope is so narrow, it can be slid past blocking structures. The endoscope also provides a wide panoramic view, whereas the microscope provides a narrower view.
Despite all the advantages and disadvantages, endoscopy is a new technology for surgical interventions, which is actively developing around the world. The German company MGB is actively working to create high-quality optics with a minimum diameter of the optical tube. A wide range of video lenses and a powerful light source help to accurately visualize the place of intervention. Choosing the endoscopic equipment of the MGB company, you choose the quality and reliability confirmed by more than 100 years of experience.
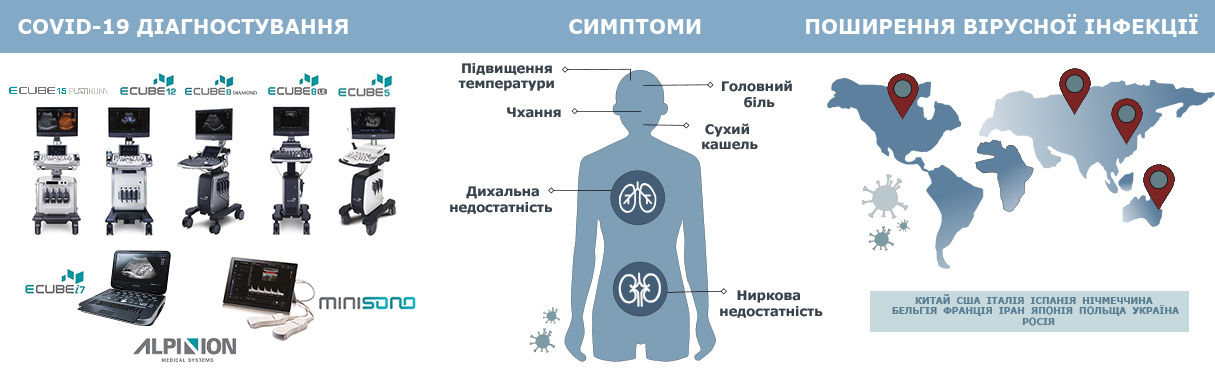
Cleaning and disinfection of ultrasonic transducers is a thorough and very important process in the operation of an ultrasonic device. So, in today's realities, in the context of the global outbreak of COVID-19, this process must be treated with extreme caution and response.
All ALPINION transducers require gentle care, cleaning and use. Extended manufacturer's recommendations are at the user manual, but we briefly recall the main thing.
This information is intended to increase user awareness of the risks of disease transmission associated with using this equipment and provide guidance in making decisions directly affecting the safety of the patient as well as the equipment user.
Diagnostic ultrasound systems utilize ultrasound energy that must be coupled to the patient by direct physical contact. Depending on the type of examination, this contact occurs with a variety of tissues ranging from intact skin in a routine exam to recirculating blood in a surgical procedure. The level of risk of infection varies greatly with the type of contact. One of the most effective ways to prevent transmission between patients is with single use or disposable devices. However, ultrasound transducers are complex and expensive devices that must be reused between patients. It is very important, therefore, to minimize the risk of disease transmission by using barriers and through proper processing between patients.
Using an inappropriate cleaning or disinfecting agent may damage the product. Cleaning products should be as close to neutral pH as possible. Any gel, cleaning or disinfectant products containing surfactants, methanol, ethanol, benzyl or methyl alcohol, bleach, methyl or ethyl paraben, polyethylene glycol, mineral oil, lubricant oil, oil based lotions, acetone, ammonia, anhydrous ammonia, iodine, iodine compounds, acids with pH5 or greater may damage or discolor your transducer.
To view recommended products from the manufacturer, see the table “Transducer Disinfectant Material Compatibility Table” list of approved products for cleaning and disinfecting ALPINION ultrasonic transducers.
What is the cleaning, disinfection and sterilization of ultrasound equipment?
Cleaning, disinfection and sterilization is a statistical decrease in the number of microbes on the surface, rather than their complete removal. As defined by the Centers for Disease Control and Prevention (CDC) [1]:
Cleaning is the removal of visible soil (eg, organic and inorganic material) from objects and surfaces and normally is accomplished manually or mechanically using water with detergents or enzymatic products.
Thorough cleaning is essential before high-level disinfection and sterilization because inorganic and organic material that remains on the surfaces of instruments interfere with the effectiveness of these processes.
Meticulous cleaning of the instrument is the key to an initial reduction of the microbial/organic load by at least 99%.1 This cleaning is followed by a disinfecting procedure to ensure a high degree of protection from infectious disease transmission, even if a disposable barrier covers the instrument during use.
The American Institute of Ultrasound in Medicine [2] and the CDC describe several levels of disinfection and sterilization:
Disinfection describes a process that eliminates many or all pathogenic microorganisms, except bacterial spores.
Low-Level Disinfection — destruction of most bacteria, some viruses, and some fungi. Low-level disinfection will not necessarily inactivate Mycobacterium tuberculosis or bacterial spores.
Mid-Level Disinfection — inactivation of M Tuberculosis, bacteria, most viruses, most fungi, and some bacterial spores.
High-Level Disinfection — destruction/removal of all microorganisms except bacterial spores.
Sterilization describes a process that destroys or eliminates all forms of microbial life and is carried out in healthcare facilities by physical or chemical methods. High-level sterilizers and disinfectants recommended by the U.S. Food and Drug Administration (FDA) [3] are listed in the table.
Sterilants and High-Level Disinfectants Listed by the FDA
| Name | Composition | Action |
| Glutaraldehyde | Organic compound (CH2(CH2CHO)2) | Induces cell death by cross-linking cellular proteins; usually used alone or mixed with formaldehyde |
| Hydrogen peroxide | Inorganic compound (H2O2) | Antiseptic and antibacterial; a very strong oxidizer with oxidation potential of 1.8 V |
| Peracetic acid | Organic compound (CH3CO3H) | Antimicrobial agent (high oxidation potential) |
| Ortho-phthalaldehyde | Organic compound (C6H4(CHO)2) | Strong binding to outer cell wall of contaminant organisms |
| Hypochlorite/hypochlorous acid | Inorganic compound (HClO) | Myeloperoxidase-mediated peroxidation of chloride ions |
| Phenol/phenolate | Organic compound (C6H5OH) | Antiseptic |
| Hibidil | Chlorhexidine gluconate (C22H30Cl2N10) | Chemical antiseptic |
Step 1: Cleaning the transducer
Cleaning is an important procedure that is carried out before disinfecting the transducer. The transducer must be cleaned after each use.
1) Disconnect the transducer from the system.
2) Moisten a clean gauze pad with purified water and wipe the transducer to remove any gel or particles remaining on the transducer. If purified water is not effective, then you can use an approved pre-cleaner or low-level disinfectant (more here).
3) Carefully wipe the entire transducer, including the cable and connector. When cleaning the connector, do not allow any type of fluid to enter through the connector strain relief, electrical contacts or areas surrounding the locking-lever shaft and the strain relief.
4) To remove remaining particulate and cleaning residue, use cleaning wipes according to the manufacturers’ instructions, or rinse thoroughly with water up to the immersion point. Do not immerse the connector, connector strain relief, or cable that is within 5 cm of the connector strain relief.
5) Dry the transducer using a sterile cloth or gauze after rinsing. Do not dry the transducer by heating it.
6) Examine the housing, strain relief, lens and seal for damage, and check for any functional problem. If any damage is found, do not use a transducer and contact your ALPINION MEDICAL service engineer or an authorized agent.
Step 2: Disinfecting the transducer
To disinfect or high-level disinfect a transducer.
1) Disconnect the transducer from the system.
2) Thoroughly clean, rinse, and dry the transducer.
3) After cleaning, choose a high-level disinfection solution compatible with your transducer. If a pre-mixed solution is used, be sure to observe the solution expiration date.
4) Disinfect or high-level disinfect the transducer by following the disinfection method recommended by the disinfection solution manufacturer (more here).
5) Rinse the transducer with plenty of sterile water to remove all chemical residues on it. Or follow the rinsing method recommended by the disinfectant manufacturer to rinse the transducer.
6) Wipe off the water on the transducer with sterile cloth or gauze after rinsing it. Do not dry the transducer by heating.
7) Examine the housing, strain relief, lens and seal for damage, and check for any functional problem. If any damage is found, do not use a transducer and contact your ALPINION MEDICAL service engineer or an authorized agent.
Step 3: Sterilizing the transducer
Sterilization of endocavity transducers may be required in some countries. Alpinion Medical Systems’ endocavity transducers meet the relevant cleaning, disinfection, and sterilization requirements in accordance with provisions of the IEC 60529.
1) Before sterilization, the transducer must be cleaned. Thoroughly clean, rinse, and dry the transducer.
2) Choose a sterilization solution compatible with your transducer. For a list of approved sterilization solution (more here).
3) Sterilize the transducer by following the sterilization method recommended by the sterilization solution manufacturer.
4) Rinse the transducer with plenty of sterile water to remove all chemical residues on it. Or follow the rinsing method recommended by the sterilization solution manufacturer to rinse the transducer.
5) Wipe off the water on the transducer with sterile cloth or gauze after rinsing it. Do not dry the transducer by heating.
6) Examine the housing, strain relief, lens and seal for damage, and check for any functional problem. If any damage is found, do not.
Transducers immersion during cleaning,disinfection and sterilization
Transducers meet Ingress Protection IPX8 of EN 60529 and IEC 60529 tothe depth of the immersion line shown in the illustration only for transducerswith the “IPX8” symbol on the connector of the transducer/ 
Figure. IPX8 immersion level
Worthknowing
To avoid damage to the transducer,observe the immersion levels indicated for each transducer type. Transducerswith the protection level IPX8 are indicated by the presence of the “IPX8”symbol on the connector of the transducer. Test Standard of IPX8: Immersion for90 minutes at a depth of 1 meter.
Remember, the more carefully youtreat ultrasonic equipment, the longer it will work for you.
P.S. We recommend that you familiarize yourselfwith the statement of the Safety Committee of the World Federation of Ultrasound Diagnostics in Medicine and Biology (WFUMB) on safe ultrasound examination and clean equipment in the context of COVID-19.
Reference:
1. «Guideline for Disinfection and Sterilization inHealthcare Facilities», 2008. The site of the Center for Disease Control:http://www.cdc.gov/hicpac/pdf /guidelines/Disinfection_Nov_2008.pdf
2. AIUM: Guidelines for Cleaning and PreparingExternal- and Internal-Use Ultrasound Transducers Between Patients, SafeHandling, and Use of Ultrasound Coupling Gel. The site of the AIUM:www.aium.org/accreditation/Guidelines_Cleaning_Preparing.pdf
3. FDA-Cleared Sterilants and High Level Disinfectantswith General Claims for Processing Reusable Medical and Dental Devices. Thesite of the FDA:https://www.fda.gov/medical-devices/reprocessing-reusable-medical-devices-information-manufacturers/fda-cleared-sterilants-and-high-level-disinfectants-general-claims-processing-reusable-medical-and
4. J.S. Abramowicz, J.M. Basseal, WFUMB PositionStatement: How toperform a safe ultrasound examination and clean equipment inthe context of COVID-19, Ultrasoundin Medicine and Biology (2020), doi:https://doi.org/10.1016/j.ultrasmedbio.2020.03.033
5. Abramowicz J.S., Basseal J. WFUMB PositionStatement: How to perform a safe ultrasound examination and clean equipment inthe context of COVID-19 (translation into Russian) // Ultrasound and FunctionalDiagnostics. 2020.No. 1. P. 12–23. DOI: 10.24835/1607-0771-2020-1-12-23. (Article in Russian)
For the safety of patients and healthcare providers fighting COVID-19, we provide the transducers cleaning & disinfection guideline. Please refer to the below and check the disinfectant material compatibility of your transducers.
Low-level disinfection
High-level disinfection
Do not dry the transducer by heating.
Download transducers disinfectant guide

Ultrasound diagnostics (USD) has become an integral part of modern medicine due to its high accuracy, safety and availability. This is an examination method that uses high-frequency ultrasound waves to create images of internal organs and tissues. Ultrasound is an extremely important tool for the diagnosis and monitoring of many diseases. Let's consider the advantages of this method in more detail.
Ultrasound examinations provide detailed images of internal organs, allowing doctors to accurately diagnose the disease. Eg:
Cardiology: Ultrasound of the heart (echocardiography) allows you to evaluate the structure and function of the heart, identify pathology of valves and other structures.
Gynecology and Obstetrics: Ultrasound is used to monitor fetal development, identify developmental abnormalities, and determine the condition of the uterus and ovaries.
Abdominal examinations: Ultrasound helps evaluate the condition of the liver, gallbladder, kidneys, pancreas, and other abdominal organs.
Thanks to high accuracy, doctors can quickly and correctly make a diagnosis, which significantly increases the effectiveness of treatment. Multifunctional ultrasound systems allow you to combine all types of examination in one device.
One of the main advantages of ultrasound is its safety. It does not use ionizing radiation like X-rays or CT scans, making it safe even for pregnant women and children. Other security aspects include:
No Harmful Effects: Ultrasound has no known harmful effects when used correctly.
Non-invasive: The examination is performed without entering the body, eliminating the risk of infections and complications associated with invasive procedures.
Speed: The ultrasound procedure takes little time and does not require special preparation of the patient.
One of the requirements of the American Institute of Ultrasound in Medicine (AIUM) is the mandatory display of thermal and mechanical indices of ultrasound examination, which increases the safety standards of conducting examinations on modern ultrasound machines.
Ultrasound is available to a wide range of patients due to the relatively low cost of equipment and procedure. This allows it to be used in various medical institutions, from large hospitals to private clinics. Benefits of accessibility include:
Cost-effective: Ultrasound is significantly less expensive than many other imaging modalities, making it accessible to patients of varying financial means.
Mobility: Modern ultrasound machines can be portable, which allows them to be used in emergency rooms or on-site medical examinations.
Wide Range of Applications: Ultrasound can be used to diagnose a variety of diseases in a variety of medical specialties, making it a versatile tool.
Today there is a wide range of ultrasound devices of different levels of expertise to suit any budget.
Ultrasound diagnostics is an indispensable tool of modern medicine due to its accuracy, safety and accessibility. It allows physicians to quickly and accurately diagnose disease, safely screen patients of all ages and health conditions, even at home, and is cost-effective and accessible to a wide range of patients. These advantages make ultrasound one of the most important diagnostic methods in modern medicine.

In modern medicine, artificial lung ventilation (ALV) devices play a crucial role in sustaining the lives of patients with various types of respiratory failure.
The basic operating principles of such devices are based on several key concepts and technologies that ensure effective and safe ventilation:
Positive Pressure Principle
The ALV device operates on the principle of creating positive pressure, which facilitates the entry of air or gas mixtures into the patient’s lungs. The device ensures that air enters the airways, preventing alveolar collapse and maintaining proper gas exchange.
Ventilation Based on Controlled Variables
Artificial lung ventilation devices use three key controlled variables that determine the ventilation modes: pressure-based ventilation, volume-based ventilation, and combined ventilation that integrates both approaches.
Pressure-Based Ventilation: In this mode, the device maintains a set level of pressure in the patient’s airways. This helps ensure proper alveolar expansion and adequate gas exchange, which is critical for patients with various respiratory pathologies. This approach helps to avoid excessive pressure on the lungs, which could lead to tissue damage.
Volume-Based Ventilation: This mode delivers a specified volume of air with each breath, allowing for control over ventilation parameters and ensuring stable gas exchange. This approach is particularly useful for patients who require maintaining a consistent tidal volume.
Combined Pressure and Volume-Based Ventilation (known as "PRVC - Pressure Regulated Volume Control"): This method combines the advantages of both previous approaches, allowing for simultaneous control of pressure and volume. It provides an adaptive approach to ventilation, where the device automatically adjusts parameters based on changes in the patient’s condition. With this mode, physicians can implement lung protection strategies, adjusting to the patient’s lung compliance with each breath, minimizing the risk of complications.
Flow Sensors
ALV devices utilize two main types of flow sensors—"Hot Wire" and "Different Pressure"—for accurate measurement of flow and pressure within the circuit.
Hot Wire Sensors, located inside the exhalation valve, operate by heating a wire and measuring temperature changes, which allows precise tracking of the gas mixture flow rate. This type of sensor provides stability and durability, which is crucial for high-quality respiratory support.
Different Pressure Sensors measure the pressure difference between two points in the respiratory circuit and are the most accurate among sensors. They can be installed either distally or proximally in the patient’s circuit, depending on the patient’s type.
To ensure optimal respiratory support conditions, ALV devices should offer the ability to select appropriate sensors depending on the patient’s type.
Modern artificial lung ventilation (ALV) devices utilize various functions and ventilation modes to provide optimal respiratory support:
Ventilation Modes: ALV systems offer a range of ventilation modes, including Continuous Mandatory Ventilation (CMV), Synchronized Intermittent Mandatory Ventilation (SIMV), and Spontaneous Ventilation (SPONT). This allows doctors to select the optimal mode according to the patient's needs, taking into account their clinical condition and the required level of respiratory support.
Ventilation Parameter Control: ALV devices continuously monitor key parameters such as airway pressure, tidal volume, respiratory rate, and more. These indicators allow physicians to adjust the ventilation mode to ensure optimal support.
Data Monitoring and Visualization: ALV devices are equipped with capabilities to display respiratory cycle graphs, trends, and color-coded signals on screens. This enables doctors to easily track respiratory dynamics and adjust ventilation parameters in real time. For example, graphical displays of spontaneous and mechanical breathing provide an accurate analysis of lung function.
Automatic Control: Modern ALV devices are equipped with automatic control functions, allowing the device to independently adapt to the changing respiratory conditions of the patient.
Safety and Accuracy: Critical aspects of safety include monitoring oxygen saturation (SpO2), volumetric capnography (VCO2), and sidestream capnography (etCO2), among other modern methods. These functions enable doctors to ensure proper oxygenation, prevent potential complications, and monitor changes in gas exchange.
Each artificial lung ventilation (ALV) system offers a range of unique features aimed at enhancing the efficiency of ventilation and ensuring comfort for both patients and medical staff. Of particular note are the ALV devices from Event Medical, designed to provide high-level support for patients weighing as little as 200 grams.
An important feature is the ability of these devices to operate both from a built-in turbine and from a centralized compressed air supply system or compressor, making them versatile for various medical settings.
Innovative approaches to patient monitoring have also become a significant part of these ALV systems. The primary objective is to implement protective ventilation strategies based on monitoring various critical indicators.
Monitoring "Driving Pressure" or real-time ventilation pressure, stress index (SI), and the impact of the ALV device on the patient optimally distributes the risk of lung injury caused by mechanical ventilation (known as Ventilator-Induced Lung Injury or VILI), such as volutrauma (lung damage due to excessive air volume) and barotrauma (damage due to excessive pressure).
A crucial aspect is the monitoring of esophageal pressure, which allows for the assessment of transpulmonary pressure and lung elasticity, key to ensuring safe ventilation.
One of the key advantages is the adaptive (intelligent) mode function, which automatically transitions from full ventilation support to spontaneous (assisted) ventilation with gradual reduction of mechanical aid from the device. This feature is particularly important in the process of weaning the patient off the ventilator.
Thanks to technological advancements, artificial lung ventilation devices are becoming increasingly accessible and safer. Today, there is a wide range of ALV systems, but the main feature is their versatility and comprehensive respiratory support, including both invasive and non-invasive ventilation for patients of all age groups.


Ultrasound diagnostics is one of the most important methods of medical imaging, widely used in gynecology. It allows doctors to obtain detailed information about the condition of internal organs and the structure of the female reproductive system without the need for surgical intervention. Ultrasound diagnostics in gynecology covers a wide range of applications, from routine examinations to assess overall health to specialized studies aimed at detecting pathologies such as:
Uterine fibroids: ultrasound helps determine the size, location, and number of fibroids, which is essential for treatment planning
Ovarian cysts: ultrasound diagnostics allow for distinguishing between functional cysts and pathological ones, such as dermoid or endometrioid cysts
Endometriosis: ultrasound can detect the presence of endometrioid cysts and lesions, aiding in the diagnosis and management of this chronic condition
Inflammatory processes: ultrasound helps detect inflammatory processes in the pelvis, such as salpingitis or pyosalpinx
Endometrial polyps: ultrasound examination helps identify polyps in the uterine cavity, which may cause abnormal uterine bleeding
Uterine anomalies: ultrasound is used to detect congenital anomalies of the uterus, such as a bicornuate uterus or a uterine septum
Uterine and ovarian cancer: ultrasound diagnostics help identify suspicious masses and determine their characteristics, important for the early detection of oncological diseases
Ectopic pregnancy: ultrasound is critical in detecting ectopic pregnancies, requiring immediate medical intervention
Polycystic ovary syndrome (PCOS): ultrasound examination helps detect characteristic changes in the ovaries associated with PCOS
In addition to detecting pathologies, ultrasound diagnostics are indispensable for monitoring treatment. It allows doctors to track changes during therapy, assess treatment effectiveness, and make timely adjustments.
The role of ultrasound diagnostics is especially significant in detecting pregnancy. Ultrasound is the primary method for confirming pregnancy and evaluating its development. In the early stages, ultrasound helps determine the implantation site of the embryo, detect ectopic pregnancy, and assess the fetal heartbeat, providing peace of mind for expectant mothers and ensuring timely medical intervention when necessary.
The advantages of ultrasound diagnostics in gynecology include the non-invasiveness of the method, safety, accessibility, and relative affordability, while offering high accuracy and speed. Ultrasound allows real-time monitoring of processes.
Modern ultrasound systems have significantly evolved with the introduction of advanced technologies that improve image quality and expand diagnostic capabilities. Ultrasound systems from Alpinion deserve special mention, utilizing cutting-edge innovations to ensure high precision and diagnostic informativeness:
Three-dimensional (3D) and four-dimensional (4D) ultrasound imaging allows for a more accurate assessment of anatomical structures, enabling detailed study of organs and tissues
Doppler imaging, including color, power, and pulse-wave Doppler, evaluates blood flow in vessels, crucial for diagnosing pregnancy complications such as placenta previa or fetal health assessment, as well as detecting vascular abnormalities and tumors
Elastography is an innovative technology that assesses tissue stiffness, useful for detecting and differentiating tumor formations, such as fibroids or malignant tumors, since different tissues have varying elasticity
Automated measurement systems significantly reduce human error and improve diagnostic accuracy. For example, algorithms for automatically measuring endometrial thickness, follicle size, fetal parameters, and more ensure consistent and accurate results
The use of high-frequency transducers provides high-resolution imaging, particularly important for examining small structures.
The integration of advanced technologies into modern ultrasound systems greatly enhances their diagnostic capabilities. These innovations enable doctors to obtain detailed and accurate images, which is key for early diagnosis, effective treatment, and monitoring of gynecological diseases and pregnancy. Thanks to these technologies, ultrasound diagnostics remain at the forefront of medical imaging, providing high-quality healthcare.
Technological progress is making ultrasound systems increasingly accessible. Today, a wide range of ultrasound machines with different levels of expertise are available to suit any budget.

Multiparametric Monitors: Your Comprehensive Patient Monitoring Solution.
Multiparametric patient monitors are indispensable tools in modern medicine, providing a comprehensive overview of vital functions. Infinium Medical's monitors, renowned for their accuracy and reliability, enable healthcare professionals to promptly assess patient conditions and respond to changes. These devices are particularly valuable in intensive care units, during surgeries, and in recovery rooms.
Particularly noteworthy are patient monitors from Infinium Medical, which are distinguished by high measurement accuracy and operational reliability. The innovative technologies incorporated into these devices ensure stable performance even in difficult clinical conditions, making them an indispensable choice for medical institutions that value quality and efficiency in monitoring.
One of the key features of modern multiparameter monitors is their modular design. It allows you to adapt the equipment to the specific needs of the patient or clinical situation, providing versatility and comprehensiveness in assessing the patient's condition.
Basic modules provide basic monitoring functions:
Electrocardiogram (ECG): assessment of cardiac activity, rhythm and conduction, identification of arrhythmias, ischemia and other pathologies
Non-invasive blood pressure (NIBP): regular blood pressure monitoring to assess hemodynamics
Blood oxygenation (saturation, SpO2): measuring the level of oxygen saturation in the blood, critical for patients with respiratory failure
Body temperature: allows timely detection of inflammatory processes or other pathological changes.
According to the availability of basic monitoring modules, continuous monitoring of blood pressure (AT or BP) is carried out, which helps to detect hypertension or hypotension in the early stages, the patient’s heart rhythm by measuring heart rate (HR) and the number of pulse waves (PR), monitoring. the patient's respiratory rate (RR or RR).
Modularity allows the integration of additional functions that increase diagnostic accuracy and simplify patient monitoring.
Invasive blood pressure monitoring (IBP) – provides accurate blood pressure measurements in critically ill patients
Lateral flow or volumetric capnography (EtCO2 and VCO2) – to assess ventilation by monitoring the level of carbon dioxide in the airways and measuring the concentration of CO2 in exhaled air
Blood gas analysis (Multi-gas) - helps evaluate acid-base balance, oxygen saturation and the concentration of anesthetics in the blood
Neuromonitoring – to monitor the functions of the central nervous system and monitor neuromuscular conduction and depth of anesthesia (DNA)
Hemodynamic monitoring - to analyze the cardiac output (CO), which reflects the efficiency of the heart and other circulatory parameters (for example, PiCCO technology)
Bispectral Index Monitoring (BIS): To monitor the depth of anesthesia and patient brain activity
Multiparameter monitors are distinguished by their ability to integrate data from various body systems to create a complete picture of the patient's condition. This allows you to:
Simultaneously assess the functions of the respiratory, cardiovascular, nervous and other systems
Identify relationships between changes in various indicators
Predict the development of critical conditions through analysis of dynamics
Use automatic alarm systems that inform about deterioration of the condition
Use automatic data analysis algorithms to quickly inform medical personnel caring for patients about critical changes.
As technology advances, multiparametric patient monitors have become an indispensable part of modern medicine. They not only enable timely detection of critical changes in bodily functions but also provide healthcare providers with tools to predict complications, especially in intensive care units, during surgeries, and in recovery. The integration of data from various bodily systems, coupled with automated data analysis algorithms, allows medical staff to gain a clear understanding of the patient's condition and make informed decisions in real-time. Thus, multiparametric monitors remain a cornerstone in enhancing the quality and safety of patient care.

In modern medicine, endoscopy plays a key role in providing quality and safe care to patients. In particular, in gynecology, it has become an indispensable tool for the diagnosis and treatment of various diseases. With the help of endoscopic technologies, doctors can perform complex manipulations with less risk to the health of patients than with traditional open operations. The minimally invasive approach not only reduces the level of trauma, but also significantly reduces recovery time after surgical interventions.
Rigid endoscopy is a modern minimally invasive method based on the use of special optical equipment for visualization and manipulation of internal organs. This approach involves inserting a rigid endoscope through small surgical incisions or natural body openings, allowing clear images of organs and tissues to be captured on a monitor. In gynecology, endoscopy has opened new horizons for effective diagnosis and treatment, as it minimizes the need for traditional open surgery. The minimally invasive approach allows the intervention to be performed through small incisions, reducing the risk of complications. High-resolution optical systems provide detailed images of internal organs, which increases the accuracy of manipulations, and modern technologies, such as electrosurgery and lasers, allow complex operations to be performed with minimal trauma.
diagnosis of pathologies (endometriosis, fibroids, adhesions);
minimally invasive surgical treatment (removal of ovarian cysts, resection of fibroids, treatment of infertility);
assessment of the condition of the reproductive organs after treatment
The hysteroscope is also used to take a biopsy, material for histological studies, which makes it possible to accurately diagnose uterine cancer and other tumor diseases.
Endoscopic equipment used in gynecology consists of several key components that ensure the doctor’s effective work in diagnosis and treatment.
Light source: High quality xenon or LED lighting for clear visualization of anatomical structures
Camera: modern high-resolution cameras (FullHD or 4K) that transmit images to the monitor screen.
2-in-1 systems: Some modern models integrate a camera and light source in one compact unit, making the equipment more convenient and mobile.
Insufflator: A device that delivers carbon dioxide into the abdominal cavity to create a surgical space.
Irrigation pump: provides irrigation of the surgical field to improve visibility during intervention.
Electrosurgical unit: used to cut tissue and coagulate blood vessels, which minimizes bleeding.
In addition to the stand, the set of instruments used for endoscopic procedures is important:
Hysteroresectoscope: instruments for removing polyps, fibroids or other pathologies in the uterine cavity. They ensure precise manipulation and low trauma.
Flexible instruments: allow complex manipulations in hard-to-reach areas, such as in cases of endometriosis or adhesions.
Surgical forceps, scissors, clamps: specialized instruments for cutting, grasping and manipulating tissue during surgery.
Modern endoscopic equipment is constantly being improved, which allows doctors to work with maximum efficiency and provide patients with high-quality medical care.
Endoscopic treatment methods in gynecology include various types of interventions, which can be classified according to the type of instrument, technique and nature of the manipulation. These methods make it possible to effectively treat various diseases with minimal risk to the patient. Let's look at the most popular of them:
1. Laparoscopy is an endoscopic method used to examine the abdominal cavity and pelvic organs using a laparoscope. This method is the main one for the surgical treatment of gynecological diseases such as:
Endometriosis – using this method, endometrioid lesions are removed.
Uterine fibroids – allows you to remove small fibroids.
Ovarian cysts – laparoscopic removal of cysts makes it possible to save the ovaries, which is especially important for women planning a pregnancy.
Adhesions - in case of obstruction of the fallopian tubes or the presence of adhesions, laparoscopy allows them to be removed or eliminated, restoring the patency of the tubes.
2. Hysteroscopy is an endoscopic method for examining and treating diseases of the uterine cavity using a hysteroscope inserted through the cervical canal. This method is considered the main one for the treatment and diagnosis of uterine diseases:
Uterine polyps – allows you to accurately detect and remove uterine polyps with minimal trauma.
Uterine fibroids (small in size, localized on the mucous membrane) - the method makes it possible to perform resection of fibroids.
Congenital anomalies of the uterus - allows you to identify defects, such as uterine septum or bicornuum, and carry out correction.
Bleeding of unknown etiology - the method allows you to investigate the cause of bleeding and perform appropriate treatment.
Miscarriages - Hysteroscopy can be useful in diagnosing problems causing miscarriages, such as uterine abnormalities or hormonal imbalances.
3. Hysteroresectoscopy is a specialized form of hysteroscopy that allows for resection and removal of tumors in the uterine cavity, such as polyps, fibroids or adhesions. This is especially important for the treatment of precancerous changes and neoplasms:
Removal of large uterine polyps.
Resection of intrauterine fibroids.
Treatment of endometrial pathologies (for example hyperplasia).
5. Robotic surgical systems
Robotic surgery is a high-precision method that uses special robotic systems. They provide greater levels of precision, comfort and safety during surgery by integrating robotic arms that perform complex surgical procedures under the supervision of a surgeon. Modern robotic systems often include elements of artificial intelligence to optimize physician movements, improve accuracy, and reduce surgeon workload. The system also provides feedback on the condition of tissues during manipulation, which helps avoid damage to important structures.
Despite its many advantages, robotic surgery still remains inaccessible to a large number of the population due to its high cost, so traditional endoscopy methods do not lose their prevalence and relevance over the years.
Endoscopic treatment methods in gynecology have significantly improved the quality of medical care due to their minimally invasiveness, accuracy and rapid recovery after surgery. female patients.

Medical equipment plays a key role in the development of the healthcare system, ensuring a high level of diagnostic accuracy, treatment efficiency and patient safety. In the modern world, high-quality medical care is impossible without the use of innovative technologies that allow doctors to act faster, more accurately and efficiently. Their introduction into clinical practice helps to optimize medical processes, increase patient satisfaction and reduce risks to their health. In this article, we will look at how modern medical equipment affects the quality of care and treatment outcomes.
Modern medicine faces numerous challenges: an increase in the number of chronic diseases, an increase in demand for quality medical services and the need to reduce medical costs. Technological advances in medicine are addressing these challenges by offering innovative solutions for diagnosing, treating and monitoring patients. For example, the development of ultrasound systems, such as portable devices for rapid diagnostics in emergency medicine, makes it possible to obtain accurate images in the shortest possible time. X-ray machines equipped with digital detectors ensure minimal patient exposure to radiation and high image quality. Rigid endoscopy, used in minimally invasive surgery, is a prime example of the use of modern technology: it allows doctors to perform complex operations minimally invasively and with high precision, which reduces risks for patients and shortens the recovery period.
The latest medical equipment helps automate many processes, which reduces risk and absorbs the human factor in routine work. Digital platforms for collecting and analyzing health data allow doctors to make more informed decisions. For example, patient monitors integrate with electronic medical records, providing continuous, rapid access to information about a patient's condition. Modern ventilators are equipped with functions for automatically adjusting ventilation parameters in accordance with the patient’s condition and significantly minimize the influence of the human factor. Dental X-rays use automated algorithms to produce high-resolution images, reducing patient exposure and providing rapid analysis of results.
Ultrasounds, X-ray machines, dental X-rays and medical image monitors are key tools for diagnosing a wide range of diseases. Thanks to high-resolution images, the integration of artificial intelligence and automated analysis, they allow doctors to quickly and accurately detect pathologies, including the slightest changes, which significantly increases the chances of successful treatment.
These technologies help not only make accurate diagnoses, but also create personalized and effective treatment plans.
Investing in advanced medical equipment allows hospitals to significantly reduce operating costs and increase resource efficiency. Using detectors to create X-ray images and medical monitors to view these images helps analyze images quickly and accurately, reducing diagnostic time and reducing the number of repeat tests due to human error. This also reduces the burden on diagnostic departments and the need for consumables. The introduction of portable ultrasound systems allows diagnostics to be carried out directly at the patient’s home or in remote regions. This minimizes the need for patient transport, reduces hospital operating costs and optimizes resource allocation, ensuring access to care where it is needed.
Modern medical technologies are designed not only with medical needs in mind, but also with an emphasis on inclusivity and convenience for patients with different physical abilities. This helps improve the quality of medical care and accessibility for all categories of the population, regardless of their characteristics or limitations.
Many of the latest medical devices take into account the needs of people with disabilities to provide them with maximum comfort during examination and treatment. For example, the convenient design of dental X-ray machines allows patients in wheelchairs to easily approach the equipment, and the ability to change the height of the table deck of X-ray diagnostic systems allows for easy movement of patients with disabilities. Moreover, the convenience of modern devices is ensured not only by the physical characteristics of the equipment, but also by ergonomic aspects that allow doctors and healthcare workers to work more efficiently. Efficiency of data processing, ease of use of interfaces and setup of devices allows you to reduce the time for procedures and diagnostics, which is important for patients with different needs.
Modern medical equipment is critical to improve the quality of healthcare services, providing accurate diagnosis and effective treatment. Innovative technologies not only reduce risk for patients, but also optimize medical processes, reducing costs. They help improve access to health care, especially for people with disabilities. Investments in such technologies improve hospital efficiency and lead to better patient outcomes.

Dermatoscopy is a modern method of examining the skin, which has become an integral part of the diagnosis of dermatological diseases. The use of dermatoscopes allows doctors to accurately assess the structure of skin formations, which significantly increases the accuracy of the diagnosis.
Dermatoscopes operate using advanced technologies that provide in-depth visual analysis of skin formations. Their work is based on three key elements: a light source, an optical system and specialized filters.
1. Light source
Dermatoscopes use powerful and uniform lighting, in particular LED light sources of different placement geometries, minimizing glare on the skin and ensuring deep penetration of light into the layers of the skin. This produces clear, detailed images that help doctors identify minute changes in skin structures.
2. Optical system
Multilayer optics provide 10-20x magnification, allowing doctors to examine structures invisible to the naked eye. This is critical for the analysis of pigment networks, vascular structures and marginal changes in skin formations.
3. Polarizing filters and contact plates
Polarized light helps doctors avoid glare and analyze deeper layers of the epidermis. Previously, for visualization in polarized mode, a special immersion liquid had to be applied to the skin, however, over time and the technological process, the need for this disappeared, and modern dermatoscopes already have a polarized examination mode in their functionality. The use of contact strips allows the clinician to examine the skin consistently and safely, reducing the risk of spreading infections, especially with non-contact examinations.
A dermatoscope significantly expands the possibilities for diagnosing skin diseases.
1. Detection of melanoma and other malignant neoplasms
Using polarized light technology and high resolution, dermatoscopes help identify asymmetries, color irregularities and structural changes characteristic of melanoma in the early stages.
2. Assessment of benign formations
Dermatoscopes allow physicians to confidently diagnose nevi, keratomas, papillomas and other benign lesions, reducing the need for biopsy.
3. Monitoring the dynamics of changes
Digital documentation adapters allow you to capture high-quality images on mobile devices or DSLR cameras, allowing you to track changes in formations over time.
4. Study of vascular formations
Using dermatoscopes, doctors can study the capillary network, detecting pathologies such as hemangiomas, telangiectasias and other vascular abnormalities.
5. Diagnosis of skin diseases
Dermatoscopy is effective in identifying conditions such as psoriasis, eczema, or fungal infections because of its ability to evaluate the structure of the superficial layers of the skin.
6. Risk forecasting
Thanks to the capabilities of analyzing structures and dynamics, dermatoscopy helps determine the likelihood of transformation of benign formations into malignant ones.
Combined with the doctor’s experience and modern technologies, dermatoscopy becomes one of the most effective non-invasive diagnostic methods in modern medicine. Modern dermatoscopes support integration with digital devices and applications (smartphones, cameras, etc.) to save images and monitor changes over time. The direction of establishing diagnoses based on the introduction of artificial intelligence is now developing.
Heine Optotechnik is a pioneer in creating the first dermatoscope. In 1989, the company introduced the world's first dermatoscope, DELTA 10, which became a real revolution in dermatology. This device provided magnification of up to 10 times without distortion, which significantly increased the accuracy of dermatological examinations of the time. Since the founding of the company in 1946, it has taken a leading position in the production of medical optics. Since then, HEINE Optotechnik has continued to innovate in the field of dermatoscopy, developing new models such as the DELTAOne, DELTA 30, DELTA 30 PRO, the classic DELTA 20T and the pocket-sized, quick-diagnosis mini 3000 LED.
With a constant commitment to improvement and innovation, HEINE Optotechnik remains at the forefront of medical technology, providing doctors and patients with high-quality and effective skin care tools.
One of the latest innovations from HEINE Optotechnik is colorSHIFT technology, which provides four levels of lighting color temperature:
1. Neutral Warm White (5300K): Highlights vascular structures, which is especially useful when studying vascular lesions such as hemangioma or telangiectasia.
2. Neutral Cool White (6500K): Provides natural light to accurately evaluate the pigmentation of skin lesions such as nevi or age spots.
3. Cool White (8300K): Helps analyze the surface structures of the skin in detail, which is useful when studying surface changes or monitoring the dynamics of skin conditions.
4. Blue Cool White (11000 K): Suitable for specialized studies where increased contrast of certain skin structures is required.
Thanks to colorSHIFT technology, doctors can optimize lighting for each specific case, which significantly expands the capabilities of dermatoscopy and increases diagnostic accuracy.
The new HEINE DELTA 30 PRO is equipped with advanced HEINE LED HQ technology, which features a unique LED geometry. Thanks to this, light penetrates into the deeper layers of the skin, forming a three-dimensional 3D image.
Accessories for dermatoscopes
Accessories for dermatoscopes play a key role in ensuring diagnostic accuracy, ease of use and expanding the functionality of devices. A modern arsenal of additional tools allows doctors to carry out diagnostics even in difficult conditions, adapting the technique to the individual needs of patients. Main types of accessories include:
• Smartphone adapters: These allow doctors to capture high-quality images of skin lesions, making it easier to document and monitor changes over time. The adapters are compatible with most modern phones and provide ease of use due to ease of installation and configuration. Such adapters allow doctors to conduct examinations and store images directly on a smartphone, which increases efficiency and ease of access to information.
For example, a universal adapter for a smartphone, compatible with different phone models, allows you to quickly and conveniently connect a dermatoscope to the device, providing high-quality images for further analysis and storage.
• DSLR Camera Adapters: Provides the most accurate, high-resolution photography of skin lesions, ideal for documenting and monitoring changes in skin lesions over time. They provide detailed images that can be stored and compared, which is important for assessing the effectiveness of treatment and identifying potential changes in the skin.
Therefore, it is undeniable that dermatoscopy is a modern, non-invasive method for early detection and monitoring of the skin, which significantly increases the accuracy of diagnosing dermatological and oncological diseases. The use of dermatoscopes allows doctors to evaluate structural changes in detail and identify malignant neoplasms in the early stages.
Modern technologies, such as powerful lighting with a specialized position of each LED, high-quality optics with the possibility of polarized examination, as well as a different arsenal of accessories for deep skin analysis, expand the capabilities of dermatoscopes, making them an indispensable tool in medical practice.

Regular-grade displays are designed for use in our daily lives and standard office environments, in other words, for activities that do not require the best visual capabilities and high levels of detail.
Medical monitors are specifically designed for diagnostic and clinical needs and their advantages are obvious compared to conventional office displays. They provide accuracy, consistency and high image quality, which is important for diagnostic accuracy. Let's look at the key advantages of medical monitors.
The job of medical professionals, particularly radiologists, is to be able to detect tiny details that go unnoticed on regular office monitors. Accurate interpretation of these details is key to the further progress of the diagnosis. Errors in interpretation can lead to a false diagnosis and serious consequences for the patient's health. Office monitors do not provide the required accuracy and detail for medical tasks. Medical monitors guarantee high image quality, which is critical for accurate diagnosis and effective treatment.
2. Wide range of colors
Medical monitors are capable of displaying up to 1 billion colors, compared to 16 million in typical office displays. With the development of technology, this difference is sure to become even greater. This wide range of colors allows even the smallest gradations to be accurately reproduced, which is critical for medical image analysis, particularly in areas such as MRI, CT and ultrasound. Thanks to this, doctors can more accurately identify pathological changes, which improves the quality of diagnosis.
3. High resolution
Medical monitors are classified by resolution (in megapixels, MP): 2MP, 3MP, 5MP and higher:
2MP (1920x1200 or 1600x1200 pixels) – suitable for general visualization.
3MP (2048x1536 pixels) – often used for CT and MRI.
5MP (2560x2048 pixels) - optimal for mammography, where maximum detail is important.
8MP (3840 x 2160 pixels), 12MP (4200x2800 pixels) – provide multimodal visualization on one screen.
This high resolution eliminates the need to zoom or pan the image, saving time and reducing eye strain for clinicians.
4. Brightness
Medical monitors provide brightness in the range from 600 to 3000 cd/m2, which is several times higher than that of office monitors (usually about 300 cd/m2). High brightness is critical for accurately recognizing image detail, especially in bright lighting conditions. In addition, medical monitors maintain brightness stability throughout their entire lifespan, ensuring consistently high visual quality.
5. Contrast
The contrast ratio of medical monitors reaches 2000:1, which is critical for accurately identifying anomalies and working with shades of gray. This high level of contrast makes it possible to clearly distinguish even the smallest details in medical images, which is especially important for diagnostic radiology, mammography and CT. In comparison, office monitors have a contrast ratio of only 500:1–700:1, which significantly limits their use for medical purposes.
6. Image uniformity
Medical monitors provide uniform brightness and accurate color reproduction across the entire screen area (LUT technology). This guarantees high image quality regardless of their location, which is a key factor for accurate diagnosis. These monitors are available in two versions:
Monochrome monitors provide higher contrast and grayscale detail. This makes them ideal for mammography and radiography, where clarity of the smallest details is critical.
Color monitors are used for multimodal examinations such as CT, MRI and ultrasound, where a wide range of colors helps accurately analyze medical images.
The choice between a monochrome and color monitor depends on the specifics of the research, but both options provide image uniformity, which is a necessary condition for high-quality diagnostics.
Medical monitors are equipped with sensors that ensure image stability and accuracy:
Front sensor: Provides auto-calibration of brightness and color according to DICOM standards.
Ambient Light Sensor: Compensates for changes in ambient light levels for optimal visualization.
Human Presence Sensor: Puts the monitor into power saving mode when the user is away and automatically turns on when returning.
Conventional monitors do not have integrated sensors, especially the front sensor for auto-brightness calibration. In addition, their brightness decreases by 30% after the first year of use and can drop by up to 50% during the second year. This creates uncertainty about the authenticity of the image displayed on a regular monitor.
8. Compliance with medical standards
Conventional office monitors do not meet the DICOM (Digital Imaging and Communications in Medicine) medical standard for brightness and contrast. They are not equipped with the necessary tools to properly view medical images, leaving users in the medical environment to manually calibrate monitors and frequently check their status. This may cause important details to be lost in images.
Medical monitors are automatically calibrated to the DICOM standard thanks to built-in sensors, ensuring accurate and stable images. Additionally, these monitors can store and track calibration measurements throughout their lifetime, ensuring long-term accuracy and reliability.
9. Durability and long warranty period from the manufacturer
Medical monitors have a much longer lifespan than office displays. Typically, these monitors come with a warranty of up to 5 years, which ensures that key parameters such as brightness, contrast and image uniformity are maintained throughout their lifespan.
JVC is the world's leading medical monitor market with 50 years of experience. The Japanese company, known for its innovative solutions, is constantly improving the technologies introduced into medical monitors to meet the needs of modern medicine. Some of them:
Unique Dynamic Gamma technology automatically analyzes each pixel of the image, determining its type and displaying it in optimal quality. If the image is monochrome (black and white - X-ray, mammography, B-mode ultrasound, CT, MRI), it is displayed with DICOM calibration, which ensures accurate grayscale reproduction. If the image is in color (pathology, histology, CT or MRI reconstruction), Gamma 2.2 calibration is used - the optimal standard for transmitting color images.
The patented ISD - Independent Sub Pixel Drive feature uses a unique approach to pixel construction. Each pixel consists of three subpixels, which on color monitors correspond to the RGB principle (red, green, blue). With this technology, JVC optimizes the use of subpixels, increasing the monitor resolution by three times. For example, a 3 MP monitor increases its resolution to 9 MP, and a 5 MP monitor to 15 MP, providing extreme detail and clarity in images.
Uniquely designed dual monitor bracket. A special bracket designed to simultaneously accommodate two monitors. Thanks to integration with Daisy Chain technology, the bracket optimizes the working space, ensuring the convenience of the doctor's work. Placing two monitors side by side, especially 5 MP models, greatly improves the ability to visualize the breast. This allows for a 2x5 MP or 10 MP equivalent diagnostic configuration, expanding the potential for accurate image analysis.
Medical monitors are a tool that ensures diagnostic accuracy, durability and compliance with medical standards. They are essential for clinical and diagnostic needs where image quality is critical for diagnosing medical images of different modalities.
X-ray diagnostic systems provide high accuracy and efficiency in diagnosing a wide range of diseases. Their use covers various fields of medicine - from traumatology and orthopedics to oncology and dentistry. Today, there are several types of X-ray diagnostic systems, including traditional analog machines, digital X-ray systems for radiography and fluoroscopy, as well as specialized devices such as computed tomography (CT) scanners and mobile X-ray units. The widespread adoption of these systems is due to their ability to quickly produce high-quality images, allowing physicians to make informed treatment decisions. At the same time, technological developments are helping to improve diagnostic accuracy, reduce radiation exposure, and expand access to quality medical care.
In addition, the convenience and ergonomics of these systems are also very important, because they have a direct impact on the efficiency of medical staff and the comfort of patients. The article discusses important aspects of ergonomics of various types of x-ray equipment, such as fixed two- and three-station systems, C-arms, portable x-ray machines and mammographs. Particular attention is paid to the functionality and adaptability of these devices to the needs of users.
Stationary x-ray diagnostic systems for 2 workstations are widely used in medical institutions for radiographic examinations. The introduction of modern ergonomic solutions makes it possible to provide more comfortable conditions for medical personnel and the procedure for conducting examinations with minimal discomfort for the patient.
Modern ergonomic advantages:
1. Motorized column movements: Using a column with motorized movements to move the tube allows for easy and precise position changes without physical effort on the part of the operator. This reduces setup time and improves positioning accuracy
2. Auto-positioning and auto-tracking: X-ray diagnostic systems with auto-positioning function automatically adjust the X-ray tube and detector in accordance with the selected type of examination. Auto-tracking allows the handset to automatically align with the detector, greatly simplifying the operator's work and minimizing errors
3. Changeable table deck height: the height-adjustable table provides additional convenience for patients with disabilities and optimal conditions for staff while working
4. Large size of the table deck: the wide table deck allows you to comfortably accommodate patients of any size and reduces the need to move them during the examination. It also improves the efficiency of medical staff
5. Digital Detector: Using digital detectors allows you to obtain high quality images with less radiation dose in a short time. In addition, it speeds up the process of data processing and image transfer to the PACS system
6. Touch interface on the collimator: integration of a touch display allows you to quickly control the focal length, tube angle and other parameters. This reduces setup time and improves positioning accuracy
7. Automatic stitching function: The stitching function combines multiple images into a single image, which is especially useful for examining large anatomical areas such as the spine or lower extremities.
X-ray diagnostic systems are designed for performing radiography and fluoroscopy; they are distinguished by a well-thought-out design and functionality, which ensures high efficiency of medical personnel and comfort for patients.
Modern ergonomic advantages:
1. Large size of the table deck: the spacious table deck provides comfortable placement for patients of different sizes and reduces the need to move them during the examination. This reduces the risk of patient injury and simplifies the work of staff
2. Table Deck Tilt ± 90 Degrees: The ability to tilt the table deck 90 degrees in any direction allows for a wide range of examinations, including real-time fluoroscopy. Deck inclination of +90° and -90° makes the system universal for any hospital room
3. Multiple screening grids with automatic change: Modern systems can be equipped with multiple screening grids that can be automatically changed depending on the type of examination. This ensures optimal image quality with minimal radiation dose to the patient
4. Dynamic Digital Flat Panel Detectors: The use of dynamic digital flat panel detectors provides high quality images with minimal radiation dose for both static and dynamic studies. This is especially important for fluoroscopy as it allows for real-time examination with maximum detail
5. Control Console: The system control console can be equipped with an intercom and a camera to monitor the patient during positioning. This makes it possible to fine-tune the system remotely, increasing the efficiency and speed of work of medical staff
C-arches are used primarily in surgery, orthopedics and interventional radiology. Their main feature is mobility and flexibility in use.
Ergonomic advantages of modern C-arches may include:
1. Compact and lightweight system: due to its compactness and low weight, the C-arch can be easily moved between operating rooms and other diagnostic rooms, which ensures its versatility and ease of use
2. Large free zone of the C-arch: C-arches with a wide free zone allow examination of patients of any size, as well as the use of the system in complex clinical situations
3. Easy movements: modern systems provide smooth and precise movements in all directions, allowing you to quickly and easily position equipment at the desired angle for examinations or procedures
4. Bi-directional laser locator: The integration of a bi-directional laser locator allows you to accurately determine the required aiming and positioning. This reduces setup time and operation time
5. Optional Viewing Station: The system can be equipped with a mobile station with monitor on the cart, providing improved examination visibility in any surgical setting.
Diagnostic room x-rays provide maximum mobility and convenience for performing diagnostic procedures directly in the patient's room. This is an ideal solution for mission-critical applications where speed and availability are key factors.
Ergonomic advantages:
1. Compact and mobile: Room systems have a compact design and are easy to move thanks to built-in wheels, allowing equipment to be quickly delivered to the patient
2. Built-in Battery Systems: Built-in battery systems make systems easier to move in healthcare settings and also allow the system to operate autonomously, allowing radiographic examinations to be performed even when electrical power is limited
3. Wireless Digital Detectors: The use of wireless detectors simplifies the imaging process and provides flexibility in positioning. It also minimizes the need for cables, which improves operational efficiency
4.Easy to operate: Intuitive interface and quick setup capabilities allow medical staff to perform procedures effectively even in difficult conditions
Modern mammographs are designed with maximum convenience for medical staff and patients in mind. Their ergonomic advantages improve diagnostic accuracy, examination comfort, and work efficiency.
Main ergonomic advantages:
1. Speed of examination: modern mammographs provide rapid acquisition of high-quality images, which significantly reduces the time a patient spends for examination. This improves comfort, especially for patients with high sensitivity to compression
2. C-arm movements: the ability to adjust the position of the C-arm over a wide range provides optimal access for different clinical cases
3. Determination of compression strength: modern systems automatically determine the optimal compression strength, which minimizes discomfort for patients and guarantees high image quality
4. Tomosynthesis and stereotactic biopsy: support for tomosynthesis technologies allows you to obtain section-by-slice images of the mammary glands for a more accurate diagnosis of tumors. The presence of a stereotactic biopsy function allows for accurate tissue sampling
5. Digital detectors: the use of digital detectors eliminates the need for additional digitizers, which speeds up the examination process and improves image accuracy
6. CAD systems: Integrated computer image analysis (CAD) systems can automatically identify suspicious areas, increasing diagnostic accuracy and making the doctor's work easier.
Modern X-ray systems demonstrate the integration of advanced technology and careful ergonomics, making them indispensable tools in providing quality health care. Their use allows not only to improve the level of diagnosis, but also to create convenient conditions for all participants in the medical process.

According to a 2018 study, acute respiratory distress syndrome (ARDS) is diagnosed in 10% of all intensive care unit (ICU) patients and 23% of intubated patients, and the mortality rate remains high.
Lung-Protective Ventilation is a key strategy for ARDS to minimize ventilator-induced lung injury. It includes the use of small tidal volumes and control of ventilation pressure (Driving Pressure).
Ventilation pressure (∆P, Driving Pressure) is calculated as the difference between plateau pressure (Pplato) and positive end-expiratory pressure (PEEP).
The studies of Amato and colleagues have been instrumental in understanding the role of ventilation pressure as a key parameter for optimizing mechanical ventilation in patients with HRDS. They showed that high ventilation pressures are associated with increased mortality.
Ventilation pressure is an indicator of global lung stress, allowing ventilation parameters to be personalized:
Correction of tidal volume, (Vt) in accordance with the compliance of the lungs and chest
Estimation of the size of the aerated part of the lungs
The eVolution 3e ULTRA has built-in tools to automatically monitor and control ventilation pressure in real time. This allows medical personnel working with the device to quickly and without additional intervention control ventilation parameters.
Main functions:
Ventilation pressure monitoring (∆P value, Driving Pressure)
Alarms when safety limits are exceeded
Tool for setting safe ventilation pressure levels (Target Tool for all ventilation modes)
Color display of the Driving Pressure safety limit line (Target Driving Pressure Line tool) on the respiratory cycle graph to evaluate ventilation pressure dynamics (user defined)

Rigid endoscopy is an indispensable method for diagnosis and treatment in many branches of medicine, especially in pediatric surgery. It allows you to obtain a clear image of the child’s internal organs and perform minimally invasive surgical interventions with minimal tissue damage.
Since the anatomical features of children differ significantly from adults, endoscopes of smaller diameter and length (2.9 mm, 270 mm) are used in pediatric practice. This avoids unnecessary injury and makes it easier to access hard-to-reach areas. The reduced size of rigid endoscopes allows the method to be used even in newborns.
One of the key aspects of pediatric rigid endoscopy is the selection of the correct instruments. Traditionally, metal trocars are used to insert the endoscope and instruments, but in pediatric practice they have significant disadvantages due to their large weight: the risk of excessive pressure on the tissue; increased likelihood of injury. The optimal choice is carbon trocars. They have much less weight, which makes the procedure safer and reduces the load on the child’s tissues. Unlike plastic trocars, which are also lightweight, carbon trocars are reusable, autoclavable, and X-ray transparent, making them an indispensable tool during any C-arch endoscopy.
Pediatric laparoscopy also uses special instruments adapted to the anatomical features of the child’s body. The main difference from analogues is the smaller diameter and length of the tool. Standard laparoscopic instruments have a diameter of 5 mm/10 mm, while in pediatrics thinner ones with a diameter of 3 mm are used, which reduces the invasiveness of the procedure.
1. Rigid endoscopy helps to significantly reduce tissue trauma
Traditional open surgeries require large incisions, which results in more tissue damage and longer recovery times. Rigid endoscopy minimizes these risks through thin instruments and small punctures.
2. Helps prevent postoperative complications.
Compared with open surgery, endoscopic procedures reduce the risk of infection, adhesions, and bleeding.
3. After minimally invasive surgical interventions, patients’ recovery is much faster.
Because the procedure is less invasive, children return to normal life more quickly, reducing the need for long hospital stays.
4. Aesthetic result
Minimal incisions reduce scarring, which is especially important for younger patients.
5. Precision of manipulations
Modern endoscopic equipment allows the doctor to obtain high-quality images of internal organs in FullHD, 4K quality, which facilitates the precise performance of surgical procedures without unnecessary injuries.
6. Reduced pain
After traditional surgeries, children often experience severe pain, requiring the use of pain medications. Endoscopic techniques significantly reduce this discomfort.
Rigid endoscopy in pediatrics is a modern, effective and safe method of diagnosis and treatment, significantly improving the quality of medical care for children. The use of specialized pediatric instruments helps reduce risks and improve the accuracy of surgical procedures. Compared to traditional open surgery, endoscopic methods provide better results, minimize complications and significantly shorten the recovery period. However, to effectively use this technique, high-quality equipment and highly qualified physicians are required.

High precision and clarity of visualization are key factors for successful medical procedures. In areas such as dentistry, surgery, dermatology, ENT practice and veterinary medicine, doctors work with the smallest anatomical structures, where even the smallest error can affect the treatment outcome.
However, traditional methods of working without optical magnification are often accompanied by increased strain on the eyes, inaccuracy and discomfort due to forced tension in the muscles of the neck and back. Over time, this can lead to fatigue, errors and decreased efficiency.
The optimal solution is to use binocular loupes in combination with high-quality lighting. They significantly improve image detail, provide high precision and allow you to maintain an ergonomically correct posture, which reduces the physical strain on the doctor.
Modern binocular loupes adapt to the needs of the user and can be attached to a glasses frame or a helmet, providing maximum comfort at work.
When choosing binocular loupes, an important aspect is the ability to customize them for a specific user. This affects the comfort of work, ergonomics of the posture and the overall efficiency of the procedures.
There are two main types of loupes:
1. TTL loupes (Through-the-Lens) - an individual approach, but less flexibility
TTL loupes have a fixed design, since their optics are built directly into the lenses of the glasses and are adjusted to individual user parameters at the manufacturing stage. This ensures ideal centering of the optics and precise correspondence to the interpupillary distance for a specific user, without the need for additional adjustments.
However, due to this individuality, loupes cannot be adapted to another user, which can be a critical factor for public health institutions or clinics where the equipment is used by different specialists. In addition, if the interpupillary distance or working conditions change over time, TTL loupes cannot be adjusted - in this case, you will have to order a new pair.
2. Adjustable Binocular Loupes – Versatility and Comfort
Binocular loupes with adjustable interpupillary distance, such as HEINE HR and HRP, offer significantly greater flexibility in use.
Key benefits:
Versatility: Loupes are suitable for different users, as the interpupillary distance can be easily adjusted.
Adaptation to working conditions: The doctor can change the parameters depending on the type of procedure.
Ergonomics: Adjustable tilt angle reduces the strain on the neck and back, maintaining the correct posture.
Adjustable loupes allow you to maintain comfort and efficiency even during complex manipulations.
2. Key parameters for choosing the right binocular loupes.
When choosing binocular loupes to ensure effective work, two main factors must be taken into account: ergonomics and optical characteristics, they determine the comfort and efficiency of the doctor. These criteria include:
Magnification – the level of image detail.
Working distance – the optimal distance between the user’s eyes and the working area.
Angle of inclination and ergonomics – important for maintaining correct posture during work.
Optics and lighting quality – affects clarity, brightness and color accuracy.
2.1. Magnification
The most commonly used magnification is 2.5x. Lower magnification promotes better hand-eye coordination, and also provides a wider field of view and greater depth of field.
2.5x magnification is universal and is suitable for both beginners and experienced medical professionals. For those with more experience, it is recommended to use higher magnifications, in particular microsurgery.
The range of HEINE loupes ranges from 2.5x to 6x, which meets the needs of various medical fields, such as dentistry, surgery and other specialties where high accuracy and image detail are critical.
Table 1. Possible areas of application depending on the magnification of binocular loupes.
Specialization | Magnification | Possible areas of application |
ENT | 2.5x | Diagnosis and treatment of the ears and nose, such as procedures in the inner ear, sinuses |
Surgery | 2.5x, 3.5x, 4.0x | Plastic and reconstructive surgeries, transplantation, wound suturing, cardiac surgeries |
Microsurgery, neurosurgery | 4.0x, 6.0x | Delicate surgical procedures, such as operations on small vessels, nerve structures, or soft tissues |
Gynecology | 2.5x, 3.5x | Basic diagnostics and visualization of small details of the cervix, etc. |
4.0x, 6.0x | Surgical manipulations on small structures, such as laser therapy or removal of neoplasms, tissue biopsy | |
Ophthalmology | 2.5x | Plastic and reconstructive surgeries, such as blepharoplasty |
Dentistry | 2.5x | Restoration, implantology, periodontal surgical procedures, as well as during teeth cleaning |
3.5x, 4.0x | Detailed restorations, such as edge preparation in endodontics | |
6.0x | Endodontics, such as root canal treatment | |
Veterinary medicine | 2.5x | Oral cavity cleaning, urinary tract surgery |
2.2. Working distance and depth of focus
The term "working distance" means the distance from the eye to the working zone at which the image becomes clear (distance from the eye to the optimal working zone). For example, taller people who work standing need a greater working distance than someone who operates or conducts an examination while sitting.
The HEINE company offers an ideal working distance (x) for each application and user from 250 mm to 520 mm. The optimal working distance (x) does not depend on the size of the loupes, but on the physical parameters of the user and the type of procedure.
Depth of focus (y) is easily defined as the difference between the nearest and farthest distances at which the object remains in focus.
The advantage of HEINE magnifiers is a high focusing depth of up to 290 mm, which allows you to choose the most ergonomic working distance.
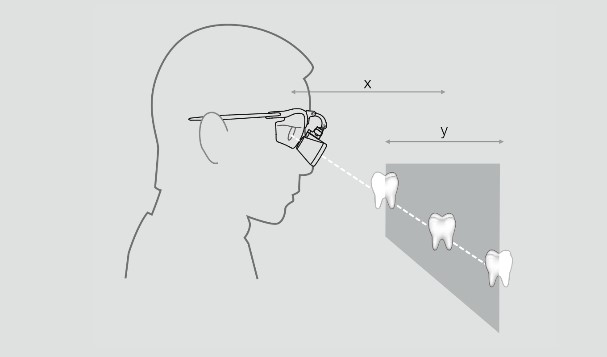
Working distance with HEINE binocular magnifiers: 340, 420 and 520 mm
2.3.1. Field of vision
HEINE magnifier systems have two key advantages: a large and balanced field of vision, as well as an optimal placement of the glasses in front of the eye. Folding systems of this type provide a wide field of view, while taking into account ergonomic requirements for comfortable work. This allows doctors to get a clear image without straining the eyes and neck.
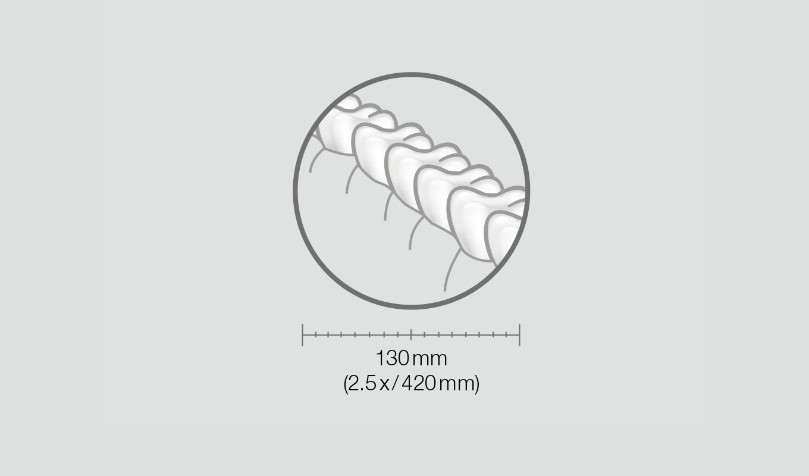
2.1. Tilt angle and ergonomics
The deviation angle is the angle between the line of sight in the normal position of the eyes and the line of sight when the user lowers the eyes. It determines how steeply or gently the optics can be adjusted in use. The optimal angle is reached when the muscles of the neck and eyes are maximally relaxed, and the head, neck and back are in a straight position.
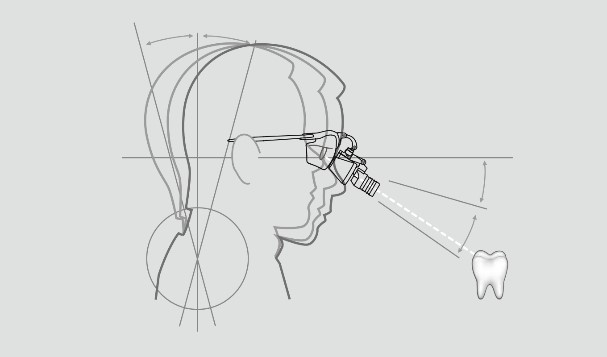
HEINE binocular magnifier systems provide maximum comfort through:
Adjustment of the angle of inclination: allows you to adjust the optics to a very steep or shallow angle, adapting it to the working needs of the user
Lightness of the design: dandruff and frames with coaxial LED lighting have a small weight, which reduces the load on the neck.
Ergonomic weight distribution: the S-shaped frame and the retaining cord evenly distribute the weight, which is important during prolonged use
Alternatively, if a headlamp is used, it must be aligned coaxially with the magnifiers, that is, their optics and light must be on the same axis relative to the field of view. This provides optimal illumination of the working area without shadows. HEINE magnifiers allow you to individually adjust the axis of the light flux in accordance with the axes of the magnifiers, which guarantees an ideal alignment of lighting in accordance with the user's preferences.
2.4. Quality of optics and lighting
2.4.1. Quality of optics
The choice of high-quality optics provides clear magnification without color distortions (rainbow effect).
HEINE HR — achromatic optics with high resolution and excellent optical properties.
HEINE HRP — prismatic optics with high resolution, provides magnification from 3.5x and the best image quality
HEINE magnifiers provide the brightest image among similar binocular models thanks to a special anti-reflective coating that reduces light reflection to 0.3%. This allows you to get extremely clear images and a wide depth of focus, ensuring optimal work without distortion even at the edges of the field of view.

2.4.2. Lighting quality
Illuminators for binocular magnifiers can be of different types, depending on the needs of the user:
Headlamps are attached to the helmet. They are usually used to provide direct and uniform illumination of the working area.
Frame-mounted illuminators are installed on magnifiers or on the frame, providing direct illumination of the inspection object.
Illuminators on the hoop - provide versatility in use and can be adjusted for optimal lighting.
High-quality LED sources provide the most natural color rendering, close to daylight. Cheap LEDs often have an excess of blue spectrum, which leads to color distortion.
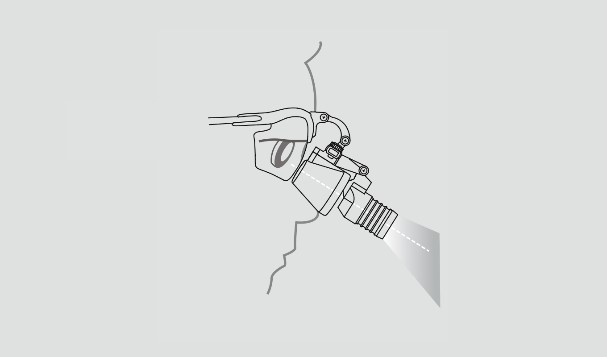
Important parameters include:
Bright and uniform illumination of the entire working field without eclipses at the edges.
Clear, bright and uniform light without glare, excluding shadows and distortions.
Lighting quality, not just a high illuminance index (lux)
The correct arrangement of the light flux - the illumination must be perfectly aligned with the binocular magnifiers for maximum consistency.
Coaxial lighting ensures the absence of shadows, illuminating hard-to-reach areas, such as cavities, thanks to the parallel arrangement of the light beam of the visual axis. Thanks to the integration of the patented HEINE LEDHQ technology, 100% coaxial, white and uniform illumination is provided.
2.4.2.1. Variants of accumulators
Battery units with cable connection are usually used for magnifiers with illumination. The optimal choice is compact and light batteries that are conveniently worn on the body without restricting movement.
Main parameters:
Charge level indicator of autonomy control.
Brightness adjustment for precise lighting adjustment.
Ease of cleaning the battery.
Power sources for loupes with forehead lighting:
Battery packs on the belt are an economical option, increased mobility and comfort.
Wireless helmet solutions - maximum freedom of movement.
The convenience of helmet-mounted wireless batteries provide conditions for dynamic work without restrictions even in complex operations.
3. Auxiliary accessories for the convenience and efficiency of working with magnifiers
For the convenience and efficiency of working with binocular magnifiers and illuminators, there are a number of useful accessories. They allow you to configure the devices in accordance with the individual needs of the user and provide additional comfort during long procedures.
Table 2. Possible accessories for binocular magnifiers and illuminators
Accessory | Description |
Polarizing filters | Polarizing filters reduce glare, increase contrast, and enhance the visibility of veins, allowing for better visibility of the upper layers of the skin. They are optional extras for some models of loupes and headlamps, allowing for more precise and comfortable work during medical procedures. |
Yellow filters | The yellow filter reduces the amount of blue light, which can be useful in dentistry to prevent premature curing of composite materials exposed to light |
Sterilized removable levers | The levers allow the loupe to be raised without removing the entire frame (bar), allowing for a quick transition between magnification and normal view, for example during patient interaction. They are removable and minimize operator contact with the loupe, improving hygiene during procedures. |
Correction frames Clip-in | Clip-in corrective frames allow prescription glasses to be integrated into binocular magnifiers, which is especially useful for people with significant vision impairment. It is recommended to use corrective frames with glasses if there are serious vision problems |
Retaining cord for eyeglass frames | The fixation cord, which is attached to the temples and pulled up behind the head, helps distribute weight evenly, ensures a stable fit, and increases comfort while wearing. |
Therefore, the use of binocular loupes and illuminators in medical practice significantly improves the accuracy and efficiency of diagnostics. The choice of high-quality optics, for example, HEINE with achromatic lenses, guarantees a clear, bright image without color distortion, which is critically important in medicine and medical interventions.
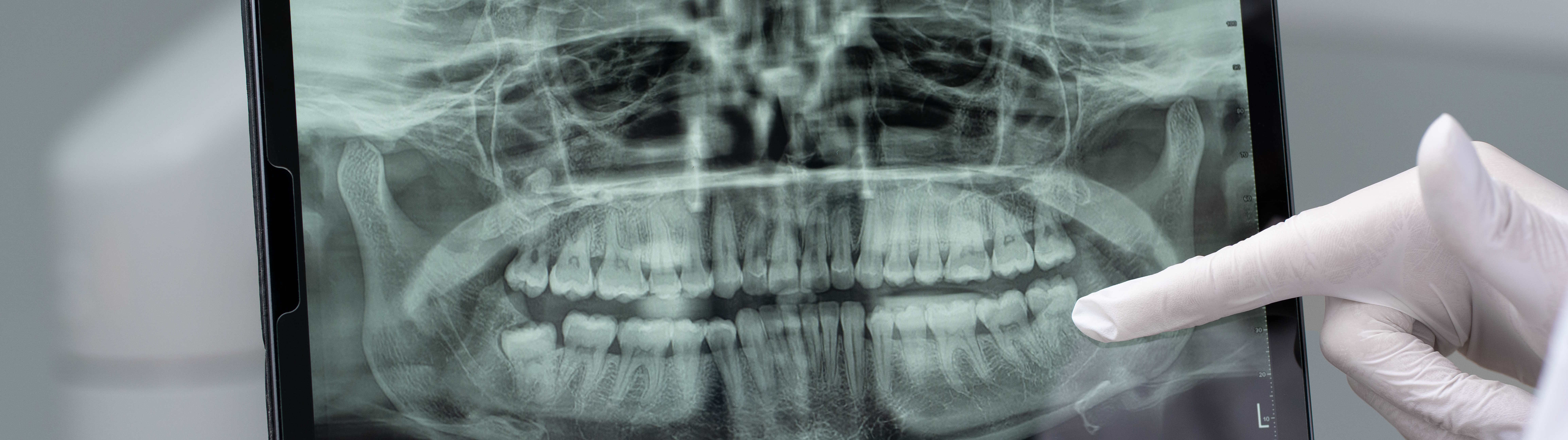
Digital devices for radiography have significantly changed the approach to diagnostics in dentistry. Previously, x-ray images in dentistry were created with the help of traditional films, which required not only a long process of obtaining images, but also significant exposure of the patient. Dentists had to manually process the films, which took a lot of time and also required additional costs for materials. In addition, at that time there was a problem with the accuracy of images, because it was not always possible to obtain sufficiently clear images for a correct diagnosis.
Technologies have changed today. Digital x-ray devices allow you to get images instantly and with minimal exposure. Modern digital sensors have replaced films, and data can be stored electronically, which greatly facilitates access to them and increases the efficiency of dentists' work. Now it is possible not only to obtain high-quality images, but also to integrate them into electronic medical systems for faster and more accurate diagnostics.
Target radiography is a method that allows you to get a picture of one or several teeth, focusing attention on a specific problem area. This method is extremely important for accurate determination of tooth disease and the subsequent appointment of individual treatment. Modern aiming pictures are as safe as possible, since the dosage of X-ray radiation is minimal.
A panoramic image of the teeth (ortopantomogram) is one of the most popular radiography methods in dentistry, which allows you to get an image of the entire jaw. This method allows the dentist to assess the general condition of teeth, bone structures and soft tissues. For detailed study, the image is displayed on a computer monitor, where the dentist can enlarge the desired areas and examine them in more detail. Modern X-ray devices provide high-quality images that allow detecting even the smallest pathologies of the dentition in the early stages. This helps to start treatment in a timely manner and prevent the development of diseases.
Cone-beam computer tomography (CPCT) is the most modern method of radiography, which allows obtaining three-dimensional 3D images of the upper and lower jaw. The high accuracy of 3D images allows you to assess the course of treatment during dental implantation, aesthetic prosthetics, and bite correction. KPKT also makes it possible to accurately determine the structure and volume of bone tissue, which is critically important for successful implantation. Pictures allow you to clearly see the position of the mandibular nerve, which helps to avoid damage during operations. This method is also used to monitor the bite correction process, providing accurate prediction of treatment results.
Digital devices for radiography in dentistry have a number of significant advantages:
Reduced exposure. With the help of digital sensors, it is possible to obtain an image with a significantly lower dose of X-ray radiation.
Image processing speed. After the examination, the image appears on the screen almost instantly, which allows you to proceed to diagnostics.
High image quality. Digital technologies allow obtaining images with high resolution, which improves the accuracy of the diagnosis.
Ease of data storage and transfer. Digital images can be stored electronically, which facilitates archiving and access to the medical history.
Environmental friendliness. There is no need to use consumables, such as film, as well as chemicals for processing films. These factors reduce the negative impact on the environment.
Stationary devices for radiography are usually used in dental clinics with a large flow of patients. They provide high image quality and are used for a wide range of diagnostic tasks.
Advantages of stationary devices:
Reliability and stability of operation: these devices are designed for continuous operation, which makes them ideal for clinics with a large flow of patients.
Increased accuracy: thanks to the use of more complex and expensive components, stationary devices are able to provide higher accuracy of images.
A wide range of uses: they can be used for various types of examinations — from standard X-ray images to computer tomography or panoramic images.
Ease of maintenance: stationary devices usually require minimal maintenance.
However, stationary devices take up more space, and their installation requires special conditions, in particular to ensure safety from X-ray radiation.
Mobile x-ray machines are becoming more and more popular due to their convenience and the ability to conduct examinations directly in the offices. They are they are ideal for emergency situations or for clinics where high mobility and efficiency in conducting examinations are necessary.
Advantages of mobile X-ray machines:
Ease of transportation: this is an excellent solution for clinics with limited space.
Speed of installation: mobile devices can be quickly set up and start research without lengthy preparation.
Flexibility in use
Although mobile devices are convenient, they have limitations in the range of applications. They are mainly suitable for basic diagnostic studies and will be ineffective for complex examinations, for example, panoramic images or computer tomography. Therefore, stationary devices are used for more detailed or specific examinations.
Digital X-ray systems have significantly improved dentistry in diagnostics and treatment. The choice between stationary and mobile equipment depends on the specifics of the clinic and the needs of patients. It is important to carefully approach the choice of equipment to ensure the best quality of service and comfort for patients.

The postoperative period in patients who have undergone surgery, especially in the chest organs, is often accompanied by the risk of developing respiratory complications. In such cases, the use of artificial lung ventilation (ALV) plays a key role in ensuring proper oxygenation, maintaining lung function and preventing complications. The choice of high-quality ALV plays a critical role in the process of patient rehabilitation, reducing complications and accelerating the recovery of lung function.
After surgery, patients often face problems such as hypoxia, atelectasis, and impaired drainage of secretions in the airways. Ensuring adequate ventilation and oxygenation is critical for patients after surgery. The main tasks of ventilators in the postoperative period are:
Maintaining adequate gas exchange - eliminating hypoxia and hypercapnia, maintaining normal levels of oxygen and carbon dioxide in the blood
Supporting respiratory mechanics - reducing the load on the respiratory muscles and controlling the inspiratory volume
Preventing atelectasis - maintaining the proper level of positive pressure in the alveoli, which prevents their collapse.
Reducing the risk of postoperative complications - such as pneumonia and respiratory distress syndrome (ARDS or GRDS).
Individual ventilation modes - using PRVC and AutoControl algorithms for adaptive control of ventilator parameters
In addition to classic control methods, such as setting the patient's lung ventilation modes, modern ventilators are equipped with additional monitoring tools that help ensure effective gas exchange and patient safety. These tools include:
Pulse oximetry
Pulse oximetry is a method of continuously monitoring blood oxygen saturation (SpO₂) and pulse rate. The pulse oximetry module for mechanical ventilation allows you to:
Assess blood oxygen saturation in real time, which is critical for monitoring the patient's respiratory function.
Detect hypoxia at an early stage, ensuring timely intervention.
Monitor the effectiveness of ventilation, helping to adjust mechanical ventilation parameters according to the patient's needs.
Capnography
Capnography is a method of measuring the concentration of carbon dioxide (CO₂) in exhaled air. There are two main types of capnography:
Volume capnography - measures the volume of CO₂ in each respiratory cycle.
Sidestream capnography - measures the concentration of CO₂ directly in the air flow.
Advantages of capnography:
Detection of ventilation disorders and assessment of the effectiveness of gas exchange.
Rapid diagnosis of respiratory failure or ventilator malfunction.
Monitor patients during anesthesia or after surgery, ensuring a safe level of ventilation.
Esophageal monitoring
Esophageal monitoring involves measuring the pressure in the esophagus using a special sensor. This allows you to estimate the transpulmonary pressure, which is the difference between the alveolar and pleural pressure. Transpulmonary pressure helps:
Assess the work of the respiratory muscles, especially the diaphragm, which is key to adjusting ventilation.
Measure the compliance of the lungs and chest, which is important for understanding the elasticity of the lungs and chest, as well as to avoid damage during ventilation.
Prevent ventilator-induced lung injury (VILI), reducing the risk of lung injury due to incorrect ventilator parameters.
Improve ventilator settings, providing more precise control of pressure and ventilation volume according to the patient's needs.
Mechanical ventilation of the lungs (MVL) can be carried out by two main methods depending on the patient's condition and the severity of respiratory failure: invasive and non-invasive ventilation. Each method has its own interfaces that ensure effective air delivery to the patient
Invasive ventilation is used in cases where the patient cannot independently maintain an adequate level of breathing. Invasive ventilation involves the use of interfaces that penetrate the patient's airways through surgical or anatomical access (endotracheal or tracheostomy tube).
The devices from Event Medical use the PRVC (Pressure Regulated Volume Control) mode, which automatically adapts the pressure to ensure a given breathing volume, which reduces the risk of barotrauma, and this measures and compares the compliance (resistance) of the lungs at each cycle.
Non-invasive ventilation is less aggressive and is used for patients who partially retain their own respiratory function. Non-invasive ventilation is performed using external interfaces (nasal cannulas, oral-nasal and full-face masks)
The innovative Slope Anasys Trigger algorithm, implemented in Event Medical devices, ensures provides adaptive selection of inspiratory triggers, which makes ventilation as comfortable as possible for the patient.
High-flow oxygen therapy in the postoperative period
High-flow oxygen therapy (HFOT) is an effective method of maintaining respiratory function in the postoperative period, especially in patients with an increased risk of respiratory complications. HFOT delivers oxygen at a rate of up to 60 L/min with an adjustable oxygen concentration (FiO up to 100%) through a high-flow nasal cannula. High oxygen flow helps to:
Increase blood oxygen saturation (SpO₂).
Reduce the work of breathing by reducing airway resistance.
Remove carbon dioxide (CO₂) from the airways, improving gas exchange.
Provide positive airway pressure, which helps maintain alveoli open.
Benefits of high-flow oxygen therapy:
Improved oxygenation even in severe forms of respiratory failure.
Reduced dyspnea and reduced load on the respiratory muscles.
Patient comfort due to heating and humidification of oxygen.
Reduced need for invasive ventilation for some patients.
Improved CO₂ removal, which is important for patients with hypercapnia.
Modern ventilators from the American company Event Medical are equipped with technologies that adapt respiratory support to the individual needs of the patient, ensuring maximum treatment efficiency and focusing on protecting the patient's lungs.
Evolution 3e Ultra with a 15-inch screen is a new and modern high-tech ventilator that supports intelligent ventilation modes and adaptive respiratory support. Thanks to advanced algorithms for automatic parameter adjustment, this device is ideal for postoperative respiratory therapy. Focused on a protective strategy for lung ventilation.
Inspiration 7i with a 17-inch screen is a ventilator that is the optimal solution for intensive care, providing high-precision control of ventilation parameters, real-time patient monitoring and an intuitive interface for doctors.
Consequently, the effectiveness of restoring lung function largely depends on the characteristics of the ventilator used. Modern models must provide accurate dosing of ventilation parameters, flexibility in setting operating modes and the ability to adapt to the needs of the patient.

Early detection of ophthalmological diseases is the key to preserving vision. Every day, ophthalmologists rely on precise and reliable instruments that allow them to detect even the smallest deviations in the structure of the eye. It is optical diagnostic instruments that ensure precision and objectivity in diagnostics, which is especially important when working with patients of all ages and with complex ophthalmological pathologies.
Optical instruments provide for examination of the fundus, assessment of the state of the retina, optic nerve, blood vessels, as well as detection of refractive anomalies. They are indispensable for primary screening, in-depth diagnostics, treatment monitoring and monitoring of chronic conditions.
It is important for an ophthalmologist to have a reliable instrument at hand that provides stable lighting, high resolution and realistic color rendition.
Types of ophthalmic instruments
HEINE Optotechnik is a pioneer in the field of ophthalmic instruments and one of the few manufacturers that maintains the entire development and production cycle exclusively in Germany, ensuring consistently high quality standards.
Direct ophthalmoscopes:
Compact, portable instruments for a quick and precise view of the fundus. They are especially convenient for work on the go or for daily use in the doctor's office.
Mini 3000 LED is a pocket ophthalmoscope with a compact design. Conveniently taken with you to on-site examinations or for use in pediatrics. Despite its size, it provides high-quality illumination with correct color rendering and clear detail thanks to reliable optics
BETA 200S LED is a professional ophthalmoscope with an extremely wide diopter range: from -36 to +38 D with a small change step (74 steps). Ideal for a thorough examination of the fundus in a clinic or office setting. A variety of apertures and filters allow the view to be easily adapted to the pupil size and type of pathology. This gives the doctor maximum flexibility in adapting to the patient. Thanks to the patented optical system with aspheric lenses and LEDHQ illumination, the BETA 200S provides unrivaled quality of view.
Indirect ophthalmoscopes (head-mounted binoculars)
Indirect ophthalmoscopes are key instruments for examining the fundus, especially with small pupils, medial opacities or retinal peripheral pathologies. Head-mounted binocular models provide a stereoscopic image and a large field of view, which allows the doctor to obtain a three-dimensional idea of the structure of the fundus. Thanks to adjustable convergence and parallax, as well as bright and homogeneous illumination, they remain indispensable both in stationary and mobile practice.
OMEGA 600 is a flagship model with revolutionary visionBOOST technology, which additionally increases the intensity of the light beam and improves contrast when examining cataracts or other types of opacities. The model has an integrated system of coordinated convergence and parallax, which adapts to small and large pupils. This ensures an optimal three-dimensional effect and precise image positioning regardless of the clinical situation. A high-tech ophthalmoscope that provides stable image quality in difficult clinical conditions - when working with narrow pupils, pediatric patients and early detection of pathologies
OMEGA 500 LED is a reliable classic model of a binocular head-mounted ophthalmoscope, which has remained the standard in daily ophthalmological practice for many years. It has high-quality optics and LEDHQ lighting, providing accurate visualization with excellent color rendition and a deep field of view
SIGMA 250 is a compact head-mounted ophthalmoscope. A portable solution for doctors who need mobility. Ideal for on-site diagnostics or work in confined spaces. Has separate convergence and parallax settings, which provides flexibility and adaptation to examination conditions with different pupil sizes
Retinoscopes
Retinoscopes are designed to objectively determine the refraction of the eye by observing the reflection of light from the retina. This is especially important for examining children, patients with communication disorders and in cases of complex ametropia. Modern models provide a clear and controllable light beam with the ability to choose between a point and linear beam.
BETA 200 LED is a retinoscope with ParaStop technology, which allows you to accurately fix a parallel beam during subjective retinoscopy. Ideal for examining refractive errors, especially in pediatric practice. Reliable design and LEDHQ lighting ensure durability and ease of use. Cards for dynamic retinoscopy are special tables with images, words, arrows, etc. They are used to assess accommodative reactions in children and adults.
Other ophthalmological instruments
There are also a number of additional ophthalmological tools that complement the daily diagnostic practice of a physician. These include:
Hand-held indirect monocular ophthalmoscopes are a compact solution for the fundus assessment
Portable slit lamps (e.g. HSL 150) are convenient tools for examining the anterior segment of the eye in the field or in a room with limited space.
Retinometers (e.g. LAMBDA 100) are tools for preliminary assessment of the visual potential in medial opacities.
Transilluminators (e.g. Finoff) are tools for diagnosing intraocular lesions, determining pupil boundaries and indirect signs of pathologies.
Ophthalmic examination lamps are sources of bright illumination for external examination of the eye.
Simulators, eye models for ophthalmoscopy and retinoscopy are used for training and practicing practical skills in clinical or educational settings.
Apertures and filters: importance for ophthalmic diagnostics
Modern ophthalmic instruments are equipped with a wide range of apertures and filters, allowing flexible adaptation of the instrument to the clinical situation, patient anatomy and examination purposes. Apertures allow the light beam to be adapted to the pupil size, lighting conditions and clinical task.
Aperture types:
Dot/small circle – optimal for small pupils and glare reduction.
Medium aperture – standard for most retinal views with medium pupil dilation.
Large aperture – used with a wide pupil for maximum field of view.
Fixation star with ruler – helps to assess central fixation in children and patients with macular pathologies.
Fixed star – used to check gaze fixation.
Slit – allows to assess the retinal relief, detect edema and detachment.
Semicircle – reduces glare and helps in assessing the periphery of the fundus.
Diffuser (usually on indirect ophthalmoscopes) – creates soft diffused lighting that is comfortable for the patient, reducing shadows and contrast.
Types of filters:
Green (red-free filter, red-free) – improves the visibility of blood vessels, nerve fibers, used to detect hemorrhages and changes in the retina.
Blue is used for examination after fluorescein, especially when examining the cornea, in particular when diagnosing epithelial defects.
Yellow – reduces the intensity of blue light, reducing light sensitivity and discomfort in patients with increased light sensitivity, especially during long-term examination.
These elements allow the doctor to more accurately assess the structures of the fundus, improve image quality and make the procedure more comfortable for the patient.
High-quality ophthalmological diagnostics begins with an accurate and reliable instrument. High-precision ophthalmic instruments with innovative technologies allow you to see more, diagnose better and help faster.

Artificial lung ventilation (ALV) is a critical technology in pediatric intensive care, allowing to support breathing in children with severe respiratory disorders. However, unlike adult patients, the use of ALV in children requires a special approach from both a technical and clinical point of view.
The respiratory system of a child differs significantly from that of an adult both anatomically and functionally:
narrow airways;
higher respiratory rate;
sensitivity to changes in pressure and volume;
risk of barotrauma and hypoventilation even with minor deviations in parameters.
Cases of using ALV in newborns and premature babies are especially difficult - any error in the settings can cause severe complications: barotrauma, hypoventilation, impaired gas exchange.
Modern pediatric ventilators have a number of specific characteristics:
Precise dosing of ventilation parameters. The inhalation volume should be very small - from 4-6 ml / kg of body weight.
Sensory sensitivity. It is important that the device "tests" each spontaneous breath of the child, without disturbing the natural rhythm.
Compatibility with non-invasive methods. In pediatrics, masks or nasal cannulas are often used, especially for stabilization.
To reduce risks and increase the effectiveness of therapy, modern ventilators have special adaptations:
Pediatric breathing circuits - reduced volume of dead space to avoid re-inhalation of CO₂.
Integrated monitoring systems - control saturation, airway pressure, respiratory rate.
Flexible software allows you to quickly change ventilation modes in accordance with the age, condition and body weight of the child.
Acoustic and visual alarm indication – given the rapid changes in the condition of small patients, the alarm system should be as informative as possible.
Children's ventilators are high-precision systems adapted to the slightest changes in the physiology of patients. The choice of the right equipment, timely adaptation of parameters and professionalism of the medical staff are the key to the safety and effectiveness of the child's treatment.
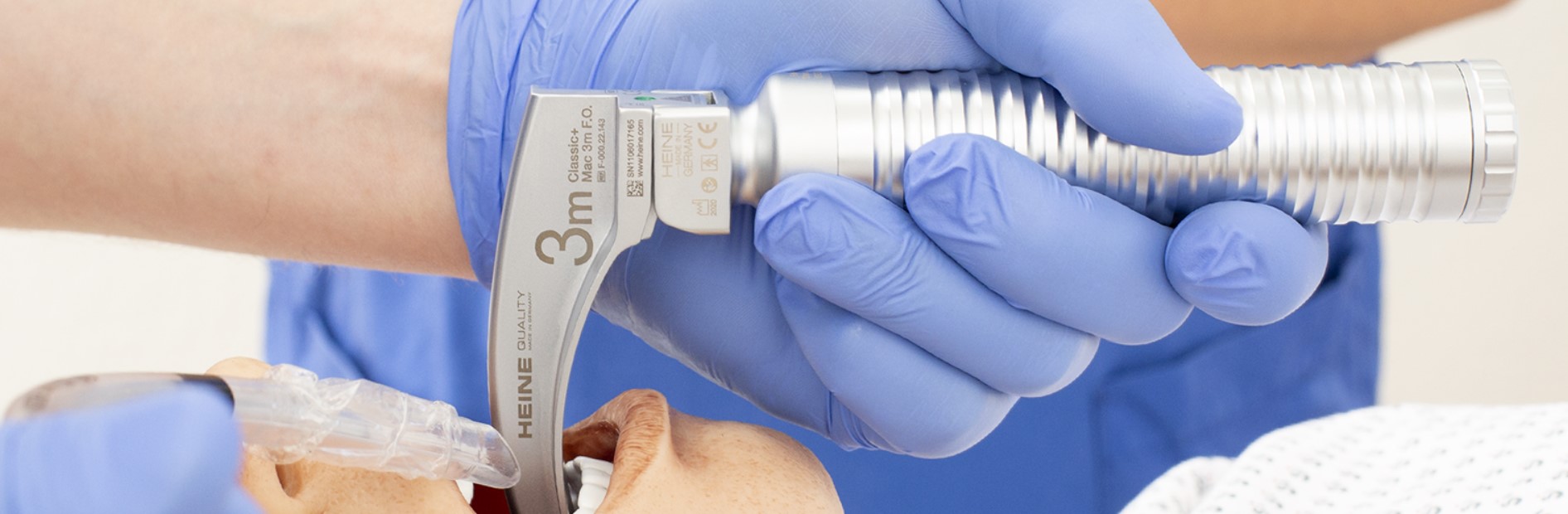
A laryngoscope is a medical instrument designed to examine the larynx and upper respiratory tract. It consists of a handle and a blade (straight or curved) with a built-in light guide that allows you to lift the epiglottis and provide an overview of the glottis. A laryngoscope is indispensable in the procedure of tracheal intubation during anesthesia, resuscitation or emergency care. The main task of the instrument is to provide a clear view of the glottis for the safe insertion of an endotracheal tube.
Modern laryngoscopes are available in two main design options with the ability to choose from different types of blades and handles - depending on the anatomical features of the patient and the conditions of clinical use:
• Classic (optical) - with direct examination through the oral cavity.
• Video laryngoscopes - modern models with an integrated miniature camera and display, allowing indirect visualization of the larynx.
Laryngoscope blades come in different shapes and sizes, allowing the instrument to be adapted to the patient's anatomical features. The most common are curved (Macintosh) and straight (Miller) blades:
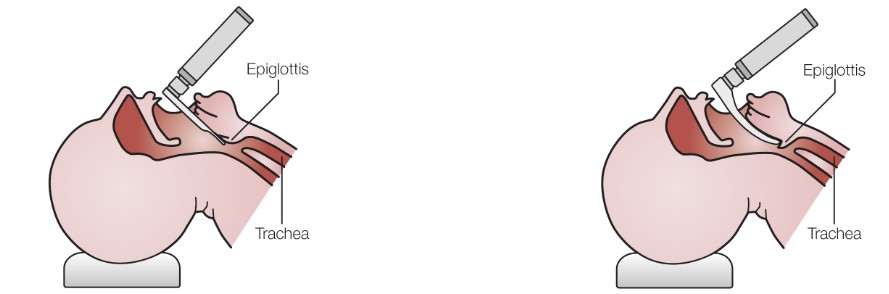
1. Straight Blade (Miller Type)
Straight blades are commonly used in neonates, children, or patients with difficult airways. The blade is inserted under the epiglottis, which is lifted by the forward movement of the laryngoscope. This provides a clear view of the vocal cords, trachea, and arytenoid cartilages.
Suggested sizes for Miller type blades:
• 00, 0 – for neonates
• 1 – for infants
• 2 – for children
• 3, 4 – for adults
2. Curved Blade (Macintosh Type)
The Macintosh is the most common blade for adults. Its tip is placed in the vallecula (anatomical depression between the base of the tongue and the epiglottis), where the glottis opens due to indirect action on the epiglottis.
Recommended sizes for Macintosh blades:
• 1 – for infants
• 2 – for children
• 3 – for adolescents and women
• 4 – for men and patients with large body mass
3. Universal pediatric blade (WIS/Paed type)
This type of blade is intuitive for users of both the Macintosh and Miller techniques and may be marked WIS or like the German company HEINE Optotechnik Classic+ Paed line. Paed type blade: a universal blade that combines the functionality of straight and curved blades and provides flexibility when intubating infant patients. The Classic+ Paed blade is suitable for both techniques - with blade placement both under the epiglottis and in the epiglottic vallecula.
Available sizes:
• Paed 0 - length 65 mm
• Paed 1 - length 78 mm
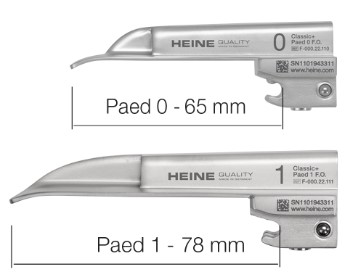
Handles act as a power source for lighting and a point of attachment for the blade. Depending on the design, lighting technology and operating conditions, they can be:
1. Reusable - designed for sterilization and repeated use. Equipped with replaceable batteries or rechargeable elements. For example:
• HEINE EasyClean LED - handles that can be sterilized without removing the lighting module. They are completely waterproof, compatible with autoclaves, as well as with low-temperature sterilization systems (STERRAD, STERIS).
• HEINE Standard F.O. - classic fiber-optic handles with the ability to use easily replaceable batteries or accumulators.
2. With a disposable shell - relevant in conditions where access to sterilization equipment is limited. After use, the shell is disposed of, ensuring quick preparation of the instrument for reuse without additional processing.
3. With integrated LED illumination – provides stable and bright light without the need to change lamps or fibers. HEINE LEDHQ technology ensures accurate color rendering, which is critical during intubation.
To adapt to various clinical scenarios, the handles are available in three standard sizes:
1. SHORT – shortened handles, convenient for intubating newborns or in limited space conditions (e.g. in neonatology or emergency medicine). They have compact dimensions and are lightweight.
2. SLIM – a thin body provides a better grip, especially convenient for users with a small hand or in conditions where maneuverability is important.
3. STANDARD – a classic full-size option for universal use in anesthesiology and resuscitation. The most autonomous option

Video Laryngoscopes and Blade Types
Video laryngoscopes integrate a miniature camera into the blade or handle, providing a clear image of the larynx on a built-in or external display. They are especially useful in cases of difficult intubation, limited visibility, and in the educational process.
Such systems can work:
• With disposable blades made of medical polymers that provide optimal rigidity and transparency, meet hygienic standards and reduce the risk of cross-infection.
• With reusable blades, which can be made of fiberglass, metal or high-quality composites. Some manufacturers use heat-resistant glass to ensure a long service life and compatibility with sterilization.
HEINE offers a modern solution - the visionPRO video laryngoscope. The uniqueness of this video laryngoscope lies in the presence of a transflective HEINE allBRIGHT display, adapting even to the brightest ambient light and intelligent image processing with realistic color rendition with HEINE LEDHQ technology. It is designed for use with disposable Macintosh blades of different sizes:
• HEINE visionPRO Macintosh disposable blades (sizes: Mac 2, Mac 3, Mac 4)
The blades have an intelligent design and the HEINE FixLock fastening system, which meets international safety standards.
• HEINE visionPRO HyMac disposable blades (sizes: HyMac 3)
Created for clinical situations where an increased angle of view of the airway is required. The blade has a reinforced curvature, which provides better visualization with complex anatomy.
HEINE Optotechnik - the standard of quality in the production of laryngoscopes
HEINE Optotechnik is one of the pioneers in the development of laryngoscopes and has been setting standards in the field of anesthesiology and resuscitation for over 75 years. High requirements for materials, German precision engineering and full control over production ensure the reliability and durability of the products.
HEINE quality is evidenced by a long warranty period:
• 10 years on HEINE Classic+ laryngoscope blades
• 5 years on complete sets (handle + blade) in the classic version
• 2 years on the HEINE VisionPRO video laryngoscope
Modern development of laryngoscopes allows you to choose the optimal instrument depending on the age, anatomy of the patient, the level of complexity of intubation and hygiene requirements. Classic reusable laryngoscope sets remain in demand in many clinics, but video laryngoscopes are becoming increasingly popular due to their functionality, safety and high level of visualization.

Modern dentistry requires effective technologies that provide patient comfort, reduce procedure time and improve the quality of treatment. The DryShield system, developed by Solmetex, is a multifunctional device for oral isolation that combines aspiration, soft tissue protection, open mouth support and patient comfort. The article discusses the principle of DryShield, its main advantages and its role in improving the efficiency of dental practice.
Isolation of the working area is critical during many dental interventions - from therapy to endodontic procedures. Traditionally, doctors use rubbers, saliva ejectors and other devices, but they often require additional personnel and do not provide comprehensive protection. In response to these challenges, the DryShield system was developed.
DryShield is an automated oral isolation system that combines several instruments in one device: a highly effective saliva ejector, an autoclavable or disposable mouthpiece, tongue, cheek and airway protection, a bite blocker and fixation of the patient's open mouth. This allows dentists to provide a dry, clean and visible working field, which contributes to the efficiency and safety of procedures.
DryShield is available as starter kits; autoclavable or disposable mouthpieces in different sizes (pediatric, small, medium, large); cleaning brushes; Y-pieces and attachments. The system is easily integrated into existing dental units, connecting directly to the High-Voltage Evacuator (HVE). This allows DryShield to be quickly adapted to the current working conditions without significant changes in the workflow.
The oral isolation system is used during:
dental restorations (especially when working with composites);
endodontic treatment;
treatment of children and patients with difficulty keeping the mouth open for long periods of time.
Versatility: the system performs the functions of several traditional instruments, reducing the need for additional equipment.
Patient comfort: soft and flexible mouthpieces provide convenience during procedures, reducing discomfort and the gag reflex.
Reduction in procedure time: the doctor focuses on manipulations, not on controlling fluid or soft tissue.
Reduction in the amount of work for the assistant: aspiration and protection occur automatically.
Reduction in the risk of aspiration of foreign objects or liquids.
Increased sterility is especially important in infection control conditions.
DryShield technology is an effective and convenient solution for modern dental practices. Its multifunctionality allows to significantly improve the working conditions of the doctor, ensure patient safety and improve the quality of treatment. Further implementation of such systems in everyday dental practice will contribute to the development of effective and patient-oriented medicine.
The artificial lung ventilation (ALV) device is the main tool in stabilizing patients with acute or chronic forms of respiratory failure.
The ALV device is necessary in the following critical conditions:
• asthmatic status;
• severe pneumonia, including COVID-19;
• traumatic brain injury that disrupts the respiratory center;
• intoxications that suppress breathing;
• postoperative period, when the patient cannot breathe on their own;
• transportation of patients in critical condition
The main goal is to maintain gas exchange while the body recovers or receives the necessary therapy.
The artificial lung ventilation system provides forced supply of oxygen-air mixture to the patient's lungs. This can be done by creating positive pressure in the airways. Modern models allow you to adjust ventilation parameters individually: volume or pressure on inspiration, respiratory rate, inhalation and exhalation ratio, PEEP level, etc.
The main ventilation modes of the Event Medical device:
1. CMV or Continuous Mandatory Ventilation (the mode is usually used when the patient is almost unable to breathe on their own). This is a type of mechanical ventilation in which the patient receives constant breathing cycles, regardless of their own respiratory attempts. In this type, the device provides the patient with breathing using a programmed frequency of respiratory cycles and inspiratory volume (Tidal Volume), which do not change even if the patient tries to breathe on their own.
2. SIMV or Synchronized Intermittent Mandatory Ventilation (the mode is used when the patient actively tries to breathe on their own): This is a type of mechanical ventilation in which the device provides the patient with a certain number of forced breathing cycles (inhalations) at a certain time, but also allows the patient to breathe on their own between these cycles. In SIMV mode, the device synchronizes the forced breaths with the patient's respiratory attempts, which avoids unwanted overlapping of artificial breaths with the patient's attempts. This can be useful for maintaining breathing in patients who are partially capable of independent breathing but still require additional support.
3. PRVC-CMV is a continuous mandatory ventilation mode by pressure and volume. In this mode, all breaths (breathing cycles) are mandatory. The ventilator helps to provide inspiration in accordance with the set respiratory rate and in response to the patient's initiated effort (switches the expiratory phase to inspiration, as in any of the CMV modes). The continuous mandatory ventilation mode with adjustable pressure and volume control (PRVC-CMV) is used to achieve optimal ventilation of the patient by providing a controlled inspiratory volume at the minimum necessary pressure. The main goal of this mode is to ensure adequate gas exchange with minimal risk of lung injury, i.e. to protect the patient's lungs during ventilation.
4. PRVC-SIMV is a synchronized intermittent mandatory ventilation mode by pressure and volume. PRVC-SIMV combines synchronized intermittent mandatory ventilation (SIMV) with pressure-regulated volume control (PRVC) described earlier. This mode provides both mandatory and spontaneous breaths, making it flexible and adaptable to a variety of clinical situations. (Similar to other SIMV modes, mandatory breaths are controlled by a set volume to be achieved (target) (VT – tidal volume), and spontaneous breaths are provided by support pressure (Psupport).
5. CPAP (Continuous Positive Airway Pressure) provides constant positive airway pressure (PEEP) in the airways throughout the entire respiratory cycle (inhalation and exhalation). The patient breathes on their own, but the machine maintains a stable pressure, which helps keep the airways open. This helps prevent airway obstruction (airways become partially or completely blocked), especially during sleep. It is often used to treat sleep apnea (a disorder in which a person’s breathing periodically stops during sleep).
6. SPAP (Spontaneous Positive Airway Pressure) is often used as a general term for ventilation modes that maintain positive airway pressure (PEEP) during the patient’s spontaneous breathing. This includes modes such as BiPAP (Bilevel Positive Airway Pressure), where there are two pressure levels. That is, SPAP = CPAP (equivalent to APRV (CareFusion) and BiLevel (Covidien) (in other ventilators)). SPAP maintains positive airway pressure during inhalation and exhalation, but the pressure can change depending on the phase of breathing (inhalation or exhalation). Provides more comfortable breathing, since the pressure during exhalation is usually lower than during inhalation, which makes exhalation easier. Often used for i treatment of patients with more severe respiratory disorders or for those who experience breathing problems even at rest.
Monitoring and visualization of data - graphical display of ventilation parameters allows doctors to track the dynamics of the patient's breathing and adjust treatment in real time.
Automatic control - modern ventilators are able to automatically adapt to changing conditions, providing accurate respiratory support in conditions of patient instability.
Safety monitoring - built-in sensors for monitoring saturation (SpO2), capnography and ventilation pressure help reduce the risk of complications such as barotrauma and volutrauma.
Modern solutions from Event Medical
Event Medical offers respiratory systems for different levels of medical practice. The devices of this brand are noted for:
• high level of autonomy - long-term operation without connection to the power grid;
• simple interface providing quick input and control of parameters;
• flexibility of ventilation modes - from basic to adaptive with pressure and volume support.
In intensive care practice, artificial lung ventilation is a decisive factor in the survival of patients with severe respiratory failure. High-tech solutions, in particular from Event Medical, allow for the most effective adaptation of artificial lung ventilation to the needs of a specific clinical case.

Modern laparoscopic surgery is rapidly developing in the direction of minimally invasive technologies with improved visualization. One of the most promising methods for increasing the accuracy of intraoperative navigation is the use of near infrared (NIR) fluorescence imaging using indocyanine green (ICG). This method allows for clear visualization of vessels, lymph nodes, tumor boundaries and organ structures in real time, which significantly improves surgical outcomes and reduces risks for patients.
Near infrared fluorescence imaging (NIR) is a modern imaging method that significantly expands the capabilities of laparoscopic surgery. It is based on the use of contrast agents that can glow in response to irradiation with light of a certain wavelength. For this, special dyes are used, in particular indocyanine green (ICG), which fluoresces in response to infrared light in the range of 750-800 nm. It is this spectral range – from 650 to 900 nm – that is called the "optical window", because biological tissues have minimal light absorption in it: hemoglobin and water almost do not interfere with the passage of rays, which allows light to penetrate to a depth of 1-2 cm. As a result, the surgeon gets the opportunity to see structures that are inaccessible under normal lighting.
After administration, ICG quickly binds to blood plasma lipoproteins and circulates in the vascular bed. Due to its size and chemical properties, the molecule does not go beyond the vessels and does not accumulate in the intercellular space. This ensures a clear, localized glow only where there are actually blood or lymphatic structures. During surgery, a laparoscopic camera equipped with an infrared light source and a sensitive sensor captures the fluorescence emitted by ICG. The resulting image is processed in real time and superimposed on a regular video image from the endoscope, forming a combined image where anatomical structures are clearly visible together with ICG-illuminated objects.
This method allows to significantly improve the visualization of important structures, in particular, vessels, bile ducts, lymph nodes, tumor borders. Due to the high signal-to-background ratio (i.e. the clarity of the glow against the background of fluorescent tissues), high precision and safety of surgical intervention are achieved. The near infrared spectrum also has minimal interference from natural tissue autofluorescence, which further increases the contrast of the image.
Indocyanine green is the only fluorescent contrast agent in the NIR range approved by the FDA for intravenous use. Due to its amphiphilic nature, the ICG molecule quickly binds to plasma lipoproteins and is distributed through the blood and tissue fluid without penetrating beyond the vascular bed. This ensures the highest specificity and safety of the method.
The main advantages of ICG:
Light penetration depth
Infrared light (650–900 nm) penetrates 1–2 cm deep into tissues — more than visible light.
Real time image
Fluorescence is displayed on the monitor during surgery without delay.
Increased safety of surgery
Allows precise detection of vessels, lymph nodes, bile ducts, tumor boundaries, etc.
The lack of tactile control is compensated by visualization.
In laparoscopy, where the surgeon does not feel the tissues with his hands, visualization provides critical information.
High signal-to-background ratio
Minimal tissue autofluorescence provides a clear, contrasting image.
• Image fusion
Fluorescent image is superimposed on regular RGB video – the surgeon sees anatomy and functional areas simultaneously.
• No additional access or probing required
Visualization is performed through existing laparoscopic ports without additional invasion.
• Suitable for various surgical areas
Hepatobiliary, oncogynecology, colorectal, thoracic, urology, assessment of anastomotic perfusion.
• High biocompatibility, low toxicity, rapid elimination.
• Stable in dry form, easy to store and prepare.
• Possibility of mass production at low cost.
• High signal-to-background ratio, which increases image contrast.
1. Hepatobiliary surgery
ICG allows visualization of liver segments, tumor outlines, vascular architecture and bile ducts. This is extremely useful in liver resections and cholecystectomies, when precise identification of the bile ducts and vessels is required.
2. Gynecological surgery
In gynecologic oncology, ICG is used for mapping lymph nodes in tumors of the cervix and body of the uterus. This allows minimizing the volume of surgical intervention and reduce the risk of complications while maintaining oncological radicality.
3. Gastrointestinal surgery
ICG is used to assess perfusion during gastric or colon resection.
It is also used to detect lymph nodes and tumors.
4. Thoracic surgery
Fluorescence imaging helps to visualize lung segments and identify lymph nodes during lung surgery.
5. Urology
During laparoscopic or robotic-assisted nephrectomy or prostatectomy, ICG allows visualization of renal vessels, urethra, and tumors, as well as lymph node dissection.
6. Detection of peritoneal metastases
ICG can help identify small foci of peritoneal metastases that are not always visible during conventional endoscopy.
The use of ICG in laparoscopic surgery is an important step in next-generation imaging. Its safety, high accuracy and ease of use make fluorescence imaging a valuable tool in both routine and oncological surgery. Combining laparoscopy with infrared fluorescence guidance allows for increased surgical precision and improved patient prognosis.

In dentistry, even the slightest inaccuracy can affect the outcome of treatment and patient safety. That is why it is so important to have a clear view of the working area and high-definition visualization during clinical and surgical interventions. Optical magnification is critical when performing complex dental procedures - from restorations to endodontic treatment. Such procedures require maximum precision, which is difficult to achieve with the naked eye. Binocular loupes have become an important tool for the modern dentist, allowing to simultaneously improve the quality of work and reduce the physical strain on the doctor.
The most common magnification for dental practice is 2.5x, which provides a wide field of view and a large depth of field. This option is optimal for daily clinical tasks: preventive examinations, restorations, periodontal interventions and hygiene procedures.
With a magnification of 3.5x, it is comfortable to work when preparing restoration edges, installing veneers or microprosthetics. For endodontics, especially when working with root canals, 4.0x or even 6.0x are used - these levels provide maximum detail, but require experience, since with magnification both the working distance and the field of view decrease.
Practical confirmation of the effectiveness of different magnifications is provided by the experience of practicing surgeons. Thus, in an interview for the professional Australian magazine "Bite magazine", Dr. Han Choi, a maxillofacial surgeon and a member of the Dental Council of New Zealand, noted that loupes with a combination of different lighting configurations significantly improve visualization and control of the surgical field, especially when working with thin tissues. In his practice, loupes with 2.5x magnification turned out to be optimal when installing implants in the area of the entire jaw, where a wide field of view is required, while he uses loupes with 3.5x for complex procedures such as guided bone regeneration (GBR) or the application of small sutures. This allows for even greater precision in tissue manipulation. According to the doctor, the use of binoculars with integrated lighting has significantly affected the quality of his daily practice, and the system itself is comfortable, lightweight and helps increase confidence during interventions.
Choosing a binocular loupe is not only a question of magnification, but also the right balance between convenience of work, field of view and depth of field. This is especially important in dentistry, where precision and long-term concentration are crucial.
According to the magnification of 2.5x, three working distance options are usually used:
340 mm - optimal for sitting work, provides a compact focus area and reduced strain on the neck.
420 mm - convenient for standing work, allows you to maintain an ergonomic posture.
520 mm - used for a narrow purpose, for example, for surgical interventions or when it is necessary to work at an increased distance.
The higher the magnification, the shorter the working distance becomes, and the field of view and depth of focus narrow. This requires greater precision, experience and gaze fixation skills from the doctor.

Premium binocular loupes are equipped with aspherical optics, which minimize optical distortion, provide high image clarity and uniform illumination across the entire field of view. This is especially important in dentistry, where accurate rendition of shape, color and texture is critical to the quality of treatment.
Image quality directly depends on the optical system. HEINE binocular loupes use advanced technologies to achieve maximum clarity without distortion:
HEINE HR — achromatic optics with high resolution, provides a clear, bright image without chromatic aberrations (rainbow effect).
HEINE HRP — prismatic optics, allowing you to achieve magnification from 3.5x and higher with maximum depth of field and detail, while maintaining correct color rendition.
Thanks to a special anti-reflective coating that reduces light reflection to 0.3%, HEINE loupes provide the brightest image among similar models, even at the edges of the field of view. This is especially important for long-term manipulations in hard-to-reach areas of the oral cavity, where even minor details are critical.

Lighting: Power, Flexibility, and Precision
The image in the loupes will not be effective without proper lighting. Dentists can choose from a variety of illuminators depending on the type of work and personal preferences:
Frame-mounted illuminators are compact, lightweight, and provide up to 50,000 lux of light. They provide coaxial illumination for everyday practice.
Hoop-mounted illuminators provide versatility of mounting and comfort during long-term work.
Headlamps on a helmet are the most powerful (up to 90,000 lux), with the ability to adjust the diameter of the light spot from 30 to 80 mm, which allows you to focus on both a large area and a point zone without losing brightness.


Heine Optotechnik battery options give the dentist the freedom to choose according to his or her working style:
mPack mini – the most compact belt-mounted battery, the lightest weight of all solutions, with up to 9 hours of battery life. Ideal for frame-mounted light configurations.
mPack – also belt-mounted, with up to 8.5 hours of battery life, ideal for headband or headband light configurations with a wired connection.
mPack UNPLUGGED – a wireless solution for mounting directly on the headband, with up to 3.5 hours of battery life, giving the dentist maximum freedom of movement and comfort during long procedures.
When mounted on the headband, the system has a balanced weight distribution, minimizing pressure on the neck and improving overall comfort. However, it should be taken into account that even with uniform weight distribution, for some users the weight of the battery on the helmet may remain noticeable, especially during long-term work. Therefore, the choice of configuration should be based on individual physical characteristics and the duration of the procedures.
Yellow filter - a useful accessory for dental practice
Special attention should be paid to the yellow filter, which can be added to the illuminator. It effectively blocks the blue spectrum of light, preventing premature hardening of composite materials during manipulations with composite materials that polymerize under the influence of the light flux.
Binocular loupes in combination with high-quality lighting and ergonomic accessories not only improve the accuracy and efficiency of dental procedures, but also significantly increase the comfort and safety of the doctor. In combination with aspherical, achromatic optics and innovative lighting, this is a modern quality standard in dentistry.

Radiography is a fundamental tool for clinical decision-making and decision-making in clinical medicine and plays a critical role in identifying and monitoring a wide range of pathological conditions, such as injuries. cartilage-subglobular system to pneumonia and leg deformities, third-party bodies, cardiovascular changes.
Traditionally, X-ray examinations are performed in inpatient diagnostic rooms, which require physical mobility or transfer from the patient's room. This is a significant part of clinical patients - especially in intensive care units, post-operative units, infectious isolation wards, intensive care units and palliative care units - є recumbent, unstable or under constant monitoring. In such cases, transportation to the X-ray room is technically difficult, but sometimes impossible.
Mobile radiography is a technological solution that allows you to monitor the patient’s bed directly. Modern mobile X-ray diagnostic systems, especially digital ones, have a high diagnostic separation capacity, high processing capability and digital integration with hospital infrastructure (PACS, RIS). This opens up new possibilities for timely diagnosis, treatment monitoring and reduction of possible risks.
There is particular interest in developing mobile X-ray systems of the Visitor T series from the Italian manufacturer Villa Sistemi Medicali, which are adapted to the needs of doctors of different levels and ensure functional flexibility diagnostic procedures.
1.1. Urgent diagnostics
In emergency departments, intensive care units, intensive care, or post-operative wards, patients are often critically ill. The movement of such patients is physiologically unsafe - through the risk of destabilization of hemodynamics, disconnection of life-safety equipment, increased stress and infection risks.
Mobile systems allow X-ray examination to be carried out directly from the patient’s bed, without changing its position. For example, a visual X-ray of the chest allows one to evaluate the leg structure, cardiac tone, placement of the endotracheal tube, central venous catheter and pleural drainage.
1.2. Speed and integration into the protocol
Mobile digital systems ensure the capture and analysis of images. This is especially important in situations that require a quick clinical decision: if there is a suspicion of pneumothorax, perforation of the intestinal tract, multiple fractures, foreign bodies, etc. Digital image processing in Visitor systems allows them to be immediately transferred to a local PACS server or displayed on a touch screen monitor for evaluation by a physician.
2.1. At the medicine shops of the secondary and tertiary regions
In municipal and regional hospitals, mobile radiographic systems are installed for servicing in a section remote from the X-ray room. This is especially true in highly specialized hospitals, where the focus on the main office outweighs the available resources. Due to its compactness and autonomy, the system can be quickly delivered to the patient, free of charge, and the results will be saved in the electronic medical system.
Visitor T30 and the digital version T30 C-DR are ideal systems when you need wide versatility and uncompromising image clarity at a low cost-effective investment. A 32 kW monoblock, which can be equipped with additional filters on the collimator, will ensure optimal display of especially foldable X-ray projections, guaranteeing high-quality images at any time.
2.2. In departments of anesthesiology and intensive care
In departments of anesthesiology and intensive care, radiography is often used or indicated several times to monitor the status of the lung, the position of catheters, the detection of pneumonia and pleural vipotu. Mobile systems will ensure a reduction in the burden on medical personnel, allow you to shorten the hour of fasting to a few minutes, and digital detectors will minimize the dose of radiation and result in a more accurate tracking of the result, and even automatically transmit it to the doctor for writing a conclusion.
In such situations, the Visitor T30 M-DR systems have proven themselves to be the most effective, as they have a high-efficiency battery system that runs an X-ray generator: this means that they do not require frequent connection to power cuts and allow for padding is practical in any place. The autonomy of the battery allows for a large exposure to various anatomical parts of the patient (approximately 400 exposures at 100 kV and 20 mAs). Moreover, the accumulators also power two large drive wheels for quick and smooth movement of the equipment, which allows the operator to easily and effortlessly handle the large distances between the medical chambers.
2.3. In infectious diseases and isolation departments
Mobile radiography has become critically important during epidemics and pandemics, especially when hospitalizing patients with viral illnesses. The placement of a mobile device directly in the isolation zone allows for the avoidance of patient transfers by the hospital and reduces the burden on staff (including the need to disinfect areas after transportation), it allows you to:
Serial caution over the dynamics of the level is lower;
assessment of the effectiveness of respiratory therapy;
defining criteria for transferring between levels of assistance (for example, from infectious diseases department to VAIT).
Digital systems T30 R-DR and T40 M-DR have a power of 32/40 kW, which is sufficient to capture a clear image of the leg, for some patients with hyperthermia, and can also implement image processing algorithms, DICOM-intelligence allows the transfer of results to an infectious disease specialist or pulmonologist in another building or warehouse - without direct contact.
2.4. Surgical and postoperative blocks
In the early postoperative period, it is important to ensure constant visual control of the patient’s position, especially with risks of postoperative bleeding, pneumonia, atelectasis and perforation. X-rays are also used to monitor the correct growth of post-operative implants (orthopedics, traumatology) and fixatives.
The advantage of the mobile system is the ability to quickly deliver the device to surgery or intensive care. This allows:
carry out control of unfastened access to the inpatient X-ray room;
minimize physical movement of the patient after general anesthesia;
It is timely to identify complications before the appearance of clinical symptoms.
high brightness of digital detectors;
automated exposure modes;
Swedes are positioned in cramped wards;
Integration with clinical information systems (PACS, RIS);
a DAP dosimeter is installed to control the dose of exposure.
4. Practical advantages in the implementation of mobile radiography
Efficiency - images are available within a few seconds after exposure.
Minimization of risks for the patient - there is no need for physical movement.
Reduced internal logistics—reduced demands on transport and personnel.
Reducing infectious risks - the reduction of infectious disease is avoided without contact with other areas of the medicine.
Digital transformation - DICOM support, snapshot archiving, remote consulting.
Mobile radiographic systems are indispensable in the practice of providing assistance to patients with difficult conditions, especially when their transportation is impossible or unsafe. They can not only change the time of diagnosis, but also improve the safety and quality of medical assistance.
Current digital systems, such as the Visitor Series T from Villa Sistemi Medicali, offer high technical productivity, adaptability to clinical minds and integration with the digital infrastructure of the medical sector. Their use in emergency care, resuscitation and infectious diseases medicine significantly improves the efficiency and safety of health care services.

Ophthalmological examination of children is one of the most important areas of diagnostic medicine. The accuracy and timeliness of diagnosis determine not only the quality of vision, but also the development of the child. Vision is a key channel for understanding the world, forming spatial orientation, coordination of movements and speech.
Unlike adults, children can be restless and have a limited ability to consciously engage in the examination process. Many congenital and early acquired pathologies occur without pronounced symptoms and remain unnoticed without a detailed instrumental examination.
In pediatric ophthalmology, carefully selected diagnostic tools are of crucial importance, ensuring an effective, fast and maximally comfortable examination. It must meet the anatomical features of the child's eye, age restrictions and behavioral reactions of young patients. High optical quality, functionality, ergonomics, reliability and the ability to flexibly adjust to each clinical situation are mandatory characteristics of modern equipment for pediatric ophthalmology.
Psychoemotional sensitivity
Children have increased sensitivity to external stimuli and often react emotionally to medical instruments, bright light or physical contact during examination. An essential condition for effective diagnostics is the creation of a calm, friendly atmosphere and the examination as delicately and quickly as possible. This approach helps minimize stress and maintain the readiness of the little patient for further examinations or treatment.
High light sensitivity
Children's eyes are especially sensitive to bright light, which can cause discomfort during examination of the fundus. Therefore, modern, for example, indirect ophthalmoscopes, are equipped with a yellow filter, softening the intensity of the light flux without reducing the quality of diagnostics.
Anatomical differences
Children's eyes are smaller in size, have a narrow pupil, and also more delicate and delicate structures - thin corneas and sclera, which requires special care during examination. In addition, the limited range of eye movements and less transparent optical media can make visualization difficult.
Therefore, ophthalmic instruments for children should provide precise adjustment of the viewing angle, a narrow beam of light, and be lightweight for the doctor's comfort.
The need for visual fixation
Children, especially those under 5 years of age, have difficulty keeping their gaze on one object for a long time. This can make it difficult to accurately examine individual areas of the retina or optic nerve. To facilitate the examination, ophthalmic instruments, such as direct hand-held ophthalmoscopes, for children are equipped with fixation targets or stars projected into the field of view, as well as other visual stimuli that hold the little patient's attention.
Dynamic retinoscopy cards
During dynamic retinoscopy and accommodation studies in children, it is especially important to maintain their visual attention, because the accuracy of the diagnosis depends on it. For this purpose, special fixation cards with simple words, bright images or geometric figures that are easy for children to perceive are used. Such cards serve as effective visual stimuli that help the child concentrate his gaze on the desired area, making the examination process more comfortable and effective.
Using parallax and convergence
Professional ophthalmological equipment, in particular binocular indirect ophthalmoscopes from the German company HEINE Optotechnik, allow you to synchronously adjust parallax and convergence. This significantly facilitates navigation during examination even with a narrow pupil, allows you to more accurately assess the three-dimensional depth of the eye structures and identify volumetric lesions, subretinal changes, neoplasms and other pathologies.
VisionBoost - additional visualization of darkened areas
The OMEGA 600 indirect ophthalmoscope is equipped with the VisionBoost function, which increases the brightness of the illumination up to 20%. This is especially important for a clear visual examination of dark areas of the fundus, such as peripheral areas or pathologically altered areas. Increased brightness thanks to VisionBoost allows the doctor to better recognize changes in the fundus, increasing the efficiency of diagnostics.
Indirect ophthalmoscopes
Monocular indirect ophthalmoscopes are convenient for quick examinations in difficult conditions, such as on-site or in emergency situations. They provide high-quality illumination and sufficient visibility, but without volumetric perception.
An indirect ophthalmoscope is an instrument that, with the help of an additional ophthalmic lens, allows the doctor to obtain a three-dimensional, stereoscopic image of the fundus. This allows to assess the depth and spatial relationships of the structures of the retina, blood vessels, optic nerve and other anatomical elements in detail. Of particular importance are binocular indirect ophthalmoscopes, which provide a detailed overview with a wide field of view even for a narrow pupil. Due to the ability to adjust convergence, parallax, as well as the presence of various apertures and filters, such devices are indispensable for accurate and comfortable examination of children.
Filters:
Green (redless) - increases the contrast of vascular structures and hemorrhages, since it absorbs red light, helping to see blood vessel pathologies more clearly.
Yellow - softens bright light, reduces patient discomfort, is especially useful for high photosensitivity of the child's eye.
Cobalt (blue) is used for fluorescence when using special dyes (for example, fluorescein), which helps to identify corneal damage.
Aperture:
A large aperture provides a wider field of view, but at the same time the light intensity is higher.
A small aperture narrows the light beam, increasing the contrast of details, which is important when examining a narrow pupil.
A diffuser diffuses the light for softer illumination, which reduces glare and discomfort.
Direct ophthalmoscopes
A direct ophthalmoscope is a compact instrument for a quick and high-quality review of the fundus. It provides an enlarged image, but without a stereoscopic effect. Its convenience in mobility and ease of use makes it indispensable for initial reviews and screening.
Modern ophthalmoscopes provide automatic integration of apertures with filters, especially green (red-free), which increases the contrast of vascular structures and improves the visibility of pathologies. Thanks to this combination, the doctor receives a clearer and more informative image even in difficult examination conditions.
Interchangeable apertures of different shapes and sizes (from large round to small pinpoint, as well as special shapes - semicircle, slit, fixation star) allow precise adaptation of the light flux and field of view to specific clinical tasks, optimizing visualization of different areas of the fundus.
One of the important functions is diopter compensation, allowing the doctor to adjust the focus depending on the refraction of the patient's eye. For example, some models have a wide correction range from -36 to +38 D with 74 adjustment steps, which ensures precise adaptation to the individual characteristics of the child's vision.
Retinoscopes
Retinoscopes are a reliable tool for objective assessment of refraction in children of all ages, including infants and children who require a special approach during examination. Due to the ability to quickly and accurately determine the refractive indices of light, retinoscopy is a key procedure for timely diagnosis and correction of visual impairment in pediatric ophthalmology. An important function of modern retinoscopes is the ability to adjust the width of the light slit - it can be increased or decreased in accordance with individual viewing needs. This allows you to adapt the illumination of the patient's eye, increasing the accuracy of measurements and convenience of the procedure.
Particularly noteworthy is the innovative ParaStop technology, which ensures fixation of a parallel beam of light during the examination. It minimizes the influence of the child's eye and head movements, which significantly increases the stability of the light beam and the accuracy of the results.
Portable slit lamps
Compact and mobile, portable slit lamps allow you to examine the anterior segment of the eye in detail without the need for stationary equipment. They are especially convenient for examining infants, young children or in conditions where space is limited - for example, in mobile or small offices. Equipped with optical filters - yellow and blue interference. Additionally, many models are equipped with a replaceable 10x magnification lens, which allows the ophthalmologist to examine the smallest structures of the eye in detail for more accurate diagnostics.
Ophthalmic hand-held examination lamps
Hand-held ophthalmic examination lamps are used for general external examination of the eye. Thanks to the soft but bright enough light, the child does not feel discomfort, which allows the doctor to carefully examine the eyelids, conjunctiva, cornea, sclera. Often used during screenings in maternity hospitals. Often used during daily visual screenings in newborns, as well as to monitor the condition of the eyelids, conjunctiva, cornea and other external structures of the eye.
Modern ophthalmic instruments, specially adapted for working with children, significantly increase the accuracy and comfort of diagnostics. They help doctors quickly identify visual impairments and promptly carry out the necessary treatment, which is important for the normal development of the child and maintaining his health.

MOT is prevention, not repair
The goal is to maintain the stable operation of the equipment and avoid breakdowns
During maintenance we:
• check the technical condition;
• calibrate and test the parameters;
• we replace worn parts;
• clean the cooling system;
• update the software and consult the user.
How often?
Recommended – 1 time per hour or after intensive use
Regular maintenance extends the service life of the equipment and prevents costly repairs

The operating table is one of the most important elements of any operating room. Not only the surgeon's comfort, but also the patient's safety depends on its design, materials and capabilities. The correct body position during the operation provides the surgeon with optimal access to the intervention area and allows the team to work without unnecessary difficulties.
Modern operating tables are made of stainless steel, which guarantees strength, durability and resistance to corrosion, even with constant contact with antiseptics and liquids. In addition, such surfaces are easy to clean and withstand repeated disinfection, which ensures a high level of hygiene and sterility.
For various knee needs, one of the most important functions of a modern operating table is the ability to accurately position the patient, so operating tables are equipped with a wide range of position adjustments: height adjustment, section tilt, headrest position and leg sections. This allows the table to be adapted for any type of intervention, from simple procedures to complex neurosurgical or orthopedic operations. Smooth movements and precise adjustment are critical so that changing the patient's position does not cause discomfort and does not distract the surgeon from work. For even greater convenience, modern operating tables are equipped with intuitive remote controls and control systems that allow you to easily and quickly adjust the table's position even during surgery. Additionally, modern operating tables are equipped with position memory and quick return to zero position functions. This allows you to save optimal settings for different types of operations and quickly restore them when used again. This feature saves time, reduces unnecessary movements and helps the team work as efficiently and confidently as possible.
At the same time, patient comfort is also of great importance, especially during long operations. Even slight pressure on human tissues can lead to pain or complications in the postoperative period, so operating tables are equipped with anatomical mattresses and special pads. They evenly distribute the load, reduce the risk of bedsores and help keep the body in a stable position throughout the procedure.
Many modern operating tables have a modular design, which allows you to select additional accessories according to the type of operation. These can be side supports, belts for fixing different parts of the body, supports for arms and legs, knee pads, various traction systems, skull clamps, etc. The use of such accessories allows you to accurately position the patient, making the operation comfortable, safe and effective.
Another important feature of modern operating tables is radiolucency, thanks to which medical personnel can perform X-ray examinations without the need to move the patient. This feature is especially valuable in orthopedics, traumatology and cardiac surgery, where the accuracy of the images directly affects the success of the operation and the safety of the patient.
Therefore, a modern operating table is a guarantee of the surgeon's comfort and patient safety. It makes any operation more precise and reliable.

Answer:
Our service engineers are always on call and ready to provide remote support.
We can remotely:
conduct initial diagnostics;
assist with equipment setup;
offer solutions without the need to go to the site.
Contact us in any convenient way - by phone or via the website

In modern medicine, patient monitors have become an indispensable tool for ensuring continuous monitoring of the patient's key vital signs. In intensive care units, operating rooms, intensive care units, and even in general wards, high-quality multiparameter monitoring allows medical staff to respond promptly to changes in the patient's condition. Thanks to the development of technology, today's patient monitors are not just devices for displaying basic indicators, but powerful analytical tools capable of integrating, processing, and predicting the state of the body in real time.
The development of medical technologies has led to the emergence of intelligent monitoring systems that combine a number of key capabilities:
High measurement accuracy
Thanks to sensitive sensors, digital signal processing, and automatic artifact compensation, monitors provide stable and clinically reliable data even in difficult conditions.
Modular architecture
Support for interchangeable modules allows you to adapt the system to specific clinical tasks - from basic observation to monitoring in the operating room, intensive care or during transportation
Intuitive interface
Clear display of parameters, optimized navigation and quick access to critical functions reduce reaction time and the risk of errors during intensive work.
Intelligent analysis algorithms and adaptive alarms
Built-in algorithms assess the dynamics of the patient's condition, reduce the number of false alarms and increase the accuracy of detecting critical events - from arrhythmias to violations of the patient's lung ventilation modes
Advanced integration capabilities
Compatibility with hospital information systems, central stations and data servers, anesthesia and respiratory machines and other systems allows for integration into a single monitoring system, real-time information transmission, remote viewing and full analysis of the received information
A modern multi-parameter patient monitor in a standard configuration provides control of key physiological parameters:
Electrocardiogram (ECG) - is a basic component for assessing cardiac activity, rhythm or conduction disturbances, helps detect arrhythmias, ischemia and other pathologies.
Non-invasive blood pressure monitoring (NIBP) is used for regular pressure monitoring, which is important for assessing hemodynamics. It shows the current state of the cardiovascular system.
Blood oxygenation (saturation, SpO2) is an assessment of the level of blood oxygen saturation, which is crucial for patients with respiratory failure. An important parameter for assessing respiratory function and oxygenation of body tissues.
Body temperature. Tracking this indicator helps to detect inflammatory processes or other pathological changes in a timely manner.
In accordance with the availability of basic monitoring modules, continuous monitoring of blood pressure (BP) is carried out, which helps to detect hypertension or hypotension in the early stages, the patient's heart rate, measuring the heart rate (HR) and the number of pulse waves (PR), monitoring the patient's respiratory rate (RR).
One of the main advantages of modern patient monitors is their modular architecture, which allows you to expand the standard configuration depending on clinical tasks. This provides high flexibility, adaptability and the ability to use one monitor in different departments of a medical institution.
Advanced cardiac monitoring:
12-lead ECG
Advanced cardiac diagnostics
Ischemic change detection
Ischemic change detection
Real-time ST segment analysis
All 12 leads can be displayed simultaneously
Arrhythmia analysis
Automatic real-time arrhythmia detection
Automatic extrasystole detection
Tachy/bradyarrhythmia detection
Atrial fibrillation/flutter detection
Heart rate variability (HRV) analysis
Assessment of autonomic nervous system function
A useful indicator for critically ill patients
Cardioversion mode
Safe operation with external defibrillators
2. Invasive hemodynamic monitoring (invasive blood pressure monitoring and related parameters):
- High accuracy at unstable hemodynamics
- Instant response to hemodynamic changes
- Fast trend display modes
- Multiple channels can be connected
Key indicators:
Invasive arterial pressure (IBP)
Central venous pressure (CVP)
Pulmonary artery pressure (PAP)
Heart chamber pressure (ICP/LVP/RVP)
Intracranial pressure (ICP)
3. Hemodynamic monitoring (to display the efficiency of the heart and other circulatory parameters):
Cardiac Output (CO) — analysis of the cardiac output indicator or minute blood volume (CHV). This is an indicator that determines the amount of blood that the heart pumps in one minute.
SV (Stroke Volume) or stroke volume (UO)
SVV (Stroke Volume Variation) - stroke volume variability.
Assessment of hemodynamic status and prediction of patient response to intravenous therapy, especially in conditions of artificial lung ventilation.
PPV (Pulse Pressure Variation) - pulse pressure variability.
Assessment of patient hemodynamic status, in particular his response to infusion therapy
SVR (Systemic Vascular Resistance) - systemic vascular resistance (SVR).
An indicator that characterizes the total resistance of blood vessels to blood flow in the body
4. Advanced monitoring of respiratory mechanics and indicators:
Capnography - assessment of lung ventilation by monitoring the level of carbon dioxide in the respiratory tract and measuring the concentration of CO2 in exhaled air:
(EtCO₂) side stream (Sidestream) or main stream (Mainstream):
Monitoring of ventilation parameters during anesthesia
Control during intubation
Early detection of hypoventilation/apnea
Volumetric (volumetric) capnography (VCO₂):
Analysis of ventilation-perfusion relationships
Assessment of respiratory efficiency
Tidal volumes (VT), minute ventilation volume (MV) for integrated or compatible modules
5. Anaesthetic gas analysis (functions include):
Automatic recognition of anesthetic agent
MAC analysis (minimum alveolar concentration)
Analysis of the inspiratory/expiratory ratio
Trends and archiving of parameters
Analysis of anesthetic gases (Multi-gas) is a key module for anesthesiology, helping to assess acid-base balance, oxygen saturation and anesthetic concentration in the blood. The Multi-Gas module can simultaneously determine the concentration of gases in the respiratory mixture: O₂ (oxygen) N₂O (nitrous oxide) CO₂ (carbon dioxide); volatile anesthetics: Isoflurane (ISO), Sevoflurane (SEVO) Desflurane (DES), Enflurane (ENF), Halothane (HAL):
6.Neuromonitoring
Bispectral Index (BIS) monitoring for monitoring the depth of anesthesia and brain activity of the patient
Anesthesia depth monitoring
Minimizing the risk of awakening during surgery
Optimizing the dose of anesthetics
NMT (neuromuscular transmission) monitoring for monitoring the functions of the central nervous system and monitoring neuromuscular conduction
Assessment of neuromuscular blockade
Control of the depth of myorelaxation during anesthesia
Specific solutions for monitoring the condition of patients
Infinium Medical (USA) is a manufacturer of high-tech patient monitors, the entire cycle of development and production of which is carried out in the USA. The company's monitor line covers all the key needs of medical institutions:
Operating — accurate multi-parameter control during surgical interventions, including anesthesia parameters.
Postoperative wards and intensive care — continuous monitoring with support for extended modules and adaptive alarms.
Bedside monitoring — stable operation and clear visualization of parameters in therapy, cardiology, etc. departments.
Patient transportation — compact models for use in ambulances or during intra-hospital transportation.
Infinium OMEGA 12 is a new generation 12.5-inch medical patient monitor on the Android platform designed to monitor and record many physiological parameters of adults, children and newborns, including both the standard ECG (electrocardiogram) monitoring configuration, heart rate, pulse oxygen saturation, pulse rate, non-invasive blood pressure, respiratory rate, temperature, and advanced monitoring parameters with the possibility of integration into the Omniview central monitoring system
Infinium OMNI III is a high-end monitor with a 15-inch high-resolution touch screen, designed to monitor and record many physiological parameters of patients of different ages, including both the standard monitoring configuration and advanced monitoring parameters with the possibility of integration into the Omniview central monitoring system. OMNI III is considered one of the most protected monitors in its class from electromagnetic interference, which increases the reliability of indicators in clinical conditions with the presence of electromagnetic interference problems.
Comprehensive approach to monitoring
Modern multi-parameter patient monitors are evolving far beyond the standard set of physiological indicators. Thanks to their flexible modular structure, they are able to support specialized monitoring: combining data from anesthesia-respiratory systems, hemodynamic indicators, anesthetic gas analysis, neurophysiological signals, etc. This approach allows you to:
Synchronously assess the functions of the respiratory, cardiovascular, nervous and other systems
Receive clinically relevant data from various sources of medical equipment (for example, anesthesia stations) on a single display.
Use algorithms that analyze the relationships between parameters, which increases the accuracy of diagnostics and prediction of changes in the condition.
Provide centralized patient monitoring even in the most complex scenarios: during operations, in intensive care units or during transportation.
Identify relationships between changes in of indicators.
Predict the development of critical conditions through the analysis of dynamics.
Use automatic signaling systems (alarms) that inform about the deterioration of the condition.
Use algorithms for automatic data analysis to quickly inform the medical staff caring for the patient about critical changes.
Conclusion
Thus, modern patient monitors are not just a tool for displaying parameters, but a clinical decision support system that enhances patient safety, optimizes staff work and ensures continuity of medical supervision

Professional installation is a complex procedure that ensures accurate, safe and stable operation of the device from the first day.
Our engineer checks the skin part, completes the adjustment, conducts tests and investigations, and instructs the staff to operate the device safely and easily.
We ensure that everything is ready so that the equipment is completely ready for work on the day of installation.
This approach will ensure more accurate results, reduce the risk of breakdowns and help eliminate the need for troublesome service calls.
Professional installation gives you peace of mind and a guarantee that your equipment will operate accurately and without interruption.

Ultrasound diagnostics is one of the key tools in pediatrics due to its safety, lack of radiation exposure, and ability to provide accurate visualization of organs in real time. For children, especially newborns and infants, ultrasound is often the method of first choice — both in routine practice and in emergency care.
Safety
Ultrasound does not use ionizing radiation, which reduces the risk of causing additional harm to the child's health. This is especially important in the dynamic monitoring of chronic diseases.
High informativeness in children
Children's organs contain more fluid and less fatty tissue, which improves the penetration of ultrasound waves and image quality. That is why ultrasound allows for a detailed assessment of structures that are less visible in adults.
Comfort and minimal stress
The procedure is painless and performed at the patient's bedside, which is especially important in intensive care units and for children with a serious general condition.
Modern ultrasound systems allow for detailed real-time imaging, which is of particular importance in pediatrics. Ultrasound provides excellent visualization of even the smallest structures, and diagnostic capabilities continue to expand due to the introduction of highly sensitive sensors, improved processing algorithms, and new scanning modes.
The use of multi-frequency sensors based on single-crystal technology deserves special attention. Single-crystal transducers generate a more powerful, uniform, and stable ultrasound signal, which allows for high-definition images at different depths. Higher sensitivity of single crystals, reduced noise and artifacts, and improved tissue contrast — all this contributes to more accurate and early diagnosis of pathologies that can progress rapidly in children.
Ultrasound diagnostics covers a wide range of clinical areas in pediatric medicine. One of the most important is neurosonography, which allows you to assess the brain structures in newborns due to the presence of a non-ossified area of the skull - the fontanel. This makes it possible to detect intracranial hemorrhages, congenital developmental anomalies, hydrocephalus and other conditions that require early intervention.
Ultrasound of the abdominal cavity is one of the most common studies in pediatrics: it allows you to visualize the liver, bile ducts, kidneys, spleen, pancreas, intestines. With the help of ultrasound, the doctor can diagnose intestinal intussusception, congenital malformations, structural abnormalities of the kidneys, acute infectious processes.
The use of ultrasound in pediatric cardiology is extremely important. Echocardiography allows you to assess the anatomy of the heart, detect congenital defects, valve disorders. Thanks to modern color, pulsed and power Doppler modes, it is possible to assess even the smallest vessels and low-velocity blood flow, which is extremely important in neonatal practice.
Ultrasound in pulmonology is another rapidly developing area. In children, it allows you to detect pleural effusions, pneumonia, atelectasis, and assess the degree of lung ventilation. Ultrasound is also indispensable in emergency care: the method allows you to quickly determine the presence of intra-abdominal fluid in injuries, assess the condition of the spleen and liver, and detect pericardial effusion or pneumothorax. In pediatric orthopedics, ultrasound is used to detect hip dysplasia, muscle and tendon pathologies after injuries, as well as inflammatory processes in the joints.
Ultrasound diagnostics in pediatrics is a universal, safe and extremely informative method, which, thanks to modern technologies, multi-frequency single-crystal sensors and high-performance ultrasound devices, allows the doctor to obtain the most accurate information about the condition of the child's body. Ultrasound today is not just a tool, but the basis for early detection of pathologies, treatment control and daily clinical decision-making in pediatric medicine.

Ultrasound diagnostics is one of the most versatile methods of medical imaging, which is dynamically developing and plays an extremely important role in modern oncology. Its importance is especially growing in the context of the global emphasis on early detection of malignant neoplasms, because timely diagnosis directly affects the choice of treatment tactics, the prognosis of patients. Ultrasound is widely used as a method of primary screening, confirmatory diagnosis and navigation of invasive procedures, which makes it an integral part of the multidisciplinary oncological approach.
One of the key advantages of the ultrasound method is its non-invasiveness and complete absence of ionizing radiation, which allows the safe use of ultrasound for multiple examinations, dynamic monitoring and screening programs, in particular in pregnant women, children and patients with chronic diseases. High availability, relatively low cost of the study, the possibility of performing in real time and portability of devices significantly expand the scope of ultrasound compared to other imaging methods. In addition, ultrasound allows for bedside imaging and rapid integration of the data into clinical decision-making.
In the context of cancer screening, ultrasound demonstrates high sensitivity in detecting structural changes in tissues at early stages of tumor development. This is especially true for breast, thyroid, liver, kidney, ovarian, prostate, and lymph node cancers. Ultrasound allows for assessment of the shape, contours, echostructure, internal heterogeneity of tumors, their relationship to surrounding tissues, and growth dynamics.
Modern ultrasound systems have significantly advanced beyond traditional grayscale imaging. An important breakthrough was the introduction of microcirculation recording technologies that allow for visualization of slow and small-diameter blood flow in vessels without the use of contrast agents. Since angiogenesis is a fundamental biological feature of malignant tumors, a detailed assessment of microvascular architecture allows to increase the accuracy of differentiation between benign and malignant formations, as well as to assess the aggressiveness of the tumor process.
An important place in modern oncological ultrasound diagnostics is occupied by elastography - a method that allows to assess the mechanical properties of tissues and, by the principle of action, brings ultrasound examination closer to the so-called "virtual palpation". The method is based on a well-known clinical principle: malignant neoplasms, as a rule, are characterized by greater stiffness compared to the surrounding unchanged tissues.
Compression (strain) elastography is based on the analysis of tissue deformation in response to external mechanical impact, which is carried out by the sensor or by the patient's natural movements (breathing, vascular pulsation). The method allows to assess the relative stiffness of tissues by comparing different areas within the zone of interest. Compression elastography has the greatest diagnostic value in the study of: thyroid gland (nodular formations), mammary glands (differentiation of benign and malignant formations), superficial lymph nodes, soft tissues, prostate gland (mainly with transrectal access). At the same time, this method is operator-dependent and has limitations in the study of deeply located organs or structures. Shear wave elastography (SWE) is based on the generation of shear waves in tissues by an ultrasonic pulse and measuring the speed of their propagation, which allows obtaining quantitative stiffness indicators (in kPa or m/s). This method is characterized by high reproducibility and less dependence on the subjective factor. Shear wave elastography is widely used in the assessment of: liver (fibrosis, cirrhosis, focal lesions), breast, thyroid, pancreas, kidneys and spleen (in selected clinical situations), tumors of various localization, in particular deep or difficult to access for compression elastography.
The use of both elastography methods in combination with B-mode and Doppler significantly increases the specificity of ultrasound diagnostics in oncology, contributes to a more accurate determination of the risk of malignancy of neoplasms, allows optimizing indications for invasive interventions and reducing the number of unfounded biopsies and false-positive diagnostic conclusions.
Contrast-enhanced ultrasound is another important tool in modern oncology. The use of ultrasound contrast agents based on microbubbles allows for a detailed analysis of the microcirculation and perfusion of tumors in real time. This opens up opportunities for accurate differential diagnosis of focal lesions, especially in the liver, kidneys and pancreas, as well as for assessing the effectiveness of chemo-, immuno- and targeted therapies by monitoring changes in tumor vascularization.
An equally important advantage of ultrasound is its role in navigating invasive procedures r. Modern functions of improved visualization of the needle allow to clearly track its position even with difficult anatomical accesses. The use of special biopsy tips, which are attached directly to the ultrasound sensor, ensures high accuracy of targeted biopsy, increases the safety of interventions and reduces the dependence of the result on the experience of the operator. This is of fundamental importance for morphological verification of the diagnosis, which remains the “gold standard” in oncology.
The key technical feature that determines the effectiveness of all the listed technologies is the use of high-quality single-crystal ultrasound sensors. Due to the homogeneous crystalline structure, such sensors provide a wider frequency range, increased sensitivity and a significantly better signal-to-noise ratio. This allows to obtain images with high spatial and contrast resolution, clearly visualize small tumor formations, microvessels and minimal changes in tissue stiffness.
Thus, ultrasound diagnostics in oncology today is not just an auxiliary method, but a full-fledged high-tech platform for screening, early detection, risk stratification and monitoring of treatment of malignant diseases. The combination of a doctor's clinical experience with modern ultrasound technologies creates the prerequisites for more accurate, safe and personalized oncological care.

Testing of medical equipment is an often necessary stage before purchase, during which the equipment is tested in real conditions of clinical practice.
It allows you to objectively assess the compliance of the equipment with the declared technical characteristics, clinical needs of the institution and operating conditions.
In the process of testing, the convenience and functionality of the equipment for medical personnel, the stability of its operation and the possibility of integration into daily work processes are also analyzed.
Based on the results of testing, conclusions are formed that are the basis for making a reasoned decision on the further purchase and implementation of medical equipment.

Diagnostics is one of the key stages of the treatment process, because the effectiveness of further treatment and the prognosis for the patient directly depend on the accuracy of the diagnosis.
Modern medicine is increasingly focused on a comprehensive approach to the diagnosis of diseases, which allows you to obtain the most complete and objective information about the state of the body. The practical necessity of such an approach is that no single examination method is able to fully reflect all structural and functional changes in the body. X-ray diagnostics remains one of the basic methods of medical imaging of internal organs and tissues, but its combination with other examination methods significantly expands diagnostic capabilities and increases the accuracy of clinical conclusions.
X-ray examinations are one of the most common and affordable methods of medical imaging. They are widely used to assess the condition of the skeletal system, respiratory organs, cardiovascular system and abdominal organs. Radiography allows you to quickly detect fractures, inflammatory processes, neoplasms and other structural abnormalities, which determines its role as an important tool for primary diagnosis. However, in some clinical cases, the data obtained need to be clarified by using additional examination methods.
Combination of radiography with ultrasound
Ultrasound examination effectively complements X-ray diagnostics, providing a more detailed assessment of the condition of soft tissues and internal organs. The combined use of X-ray and ultrasound provides comprehensive information about anatomical and functional changes, which is especially important in diseases of the abdominal cavity, genitourinary system and endocrine pathology. This approach increases the informativeness of the examination and contributes to a more accurate clinical interpretation of the results.
Radiography in combination with CT and MRI
Computed tomography and magnetic resonance imaging are used as clarifying diagnostic methods in cases where X-ray data are insufficient for a complete assessment of the condition of organs and tissues. CT allows for layer-by-layer visualization of anatomical structures and accurate determination of the localization and spread of pathological changes. MRI provides high information content in the study of soft tissues and allows assessing the condition of organs without radiation exposure. The combination of these methods with X-ray diagnostics increases the accuracy of diagnostic conclusions and the validity of clinical decisions.
Invasive X-ray methods with contrast
Contrast X-ray examinations allow for a detailed assessment of the shape, patency and functional state of hollow organs and vessels. These include angiography, urography, irrigoscopy, hysterosalpingography and other methods. The use of contrast agents significantly increases the diagnostic information content of X-ray diagnostics, especially when stenoses, obstructive processes or congenital anomalies are suspected.
Combination of X-ray with endoscopic methods
Endoscopic examination methods organically complement X-ray diagnostics, providing a more detailed assessment of the condition of internal organs. X-ray examinations allow to obtain a general idea of the anatomical changes, shape and patency of hollow organs, while endoscopy allows to directly examine the mucous membrane, to detect inflammatory processes, ulcerative lesions or neoplasms. The combination of these methods is advisable in the diagnosis of diseases of the gastrointestinal tract, respiratory tract and other systems, where it is important to assess both the structure of the organ and the condition of its inner surface.
Combination of radiography with laboratory and functional methods
X-ray diagnostics is effectively combined with other examination methods, which allows to obtain more detailed information about the patient's condition. An important component of comprehensive diagnostics are laboratory research methods that supplement the results of X-ray diagnostics with objective indicators of the functional state of the body.
Blood, urine, biochemical and immunological tests allow to detect inflammatory, infectious, metabolic and oncological processes that do not always have clear radiological signs in the early stages. Electrophysiological methods, such as electrocardiography and echocardiography, expand the possibilities of assessing the cardiovascular system, and in lung diseases, radiography in combination with spirometry and laboratory indicators of inflammation provides more accurate differential diagnosis and control of treatment effectiveness.
Advantages of an integrated approach to diagnostics
The integrated use of X-ray diagnostics in combination with other examination methods allows to significantly increase the accuracy of diagnosis, ensure early detection of pathological changes and reduce the likelihood of diagnostic errors. The combination of different diagnostic approaches allows to obtain more complete information about the course of the disease, taking into account both anatomical, as well as functional features of the pathological process. At the same time, the rational use of diagnostic methods contributes to the optimization of the examination, reduction of radiation exposure to the patient and effective use of medical resources. As a result, a holistic clinical picture is formed, which allows the doctor to choose the optimal treatment tactics in accordance with modern medical standards.

Today, more than 70% of medical diagnoses are based on laboratory test results. In large centers, laboratory technicians face critical workloads, which increases the risk of errors due to the human factor. Innovative laboratory equipment transforms the laboratory from a point of analysis collection to an intelligent center with full automation.
Modern systems solve the main concerns of doctors: low sample processing speed and insufficient reproducibility of results. Digitalization of analytical stages allows us to reach the level of personalized medicine. Now each analysis becomes the foundation for prompt therapy.
Blood biochemistry is one of the most technologically complex stages of diagnostics. The main problem here is the instability of results when working with low concentrations of analytes. BioSystems automatic biochemical analyzers solve this problem thanks to precision mechanics and closed optical systems.
Laboratory owners are often concerned about the high cost of maintaining equipment. BioSystems equipment (in particular the BA 200 and BA 400 series) optimizes costs due to the following solutions:
• Accurate dosing: the system measures the reagent in increments of 0.1 μl, minimizing its excess consumption.
• Stability of optical density: patented LED technology does not heat the reaction mixture, which guarantees the accuracy of the result throughout the shift.
• Minimum reaction volume: the ability to work with a volume of 180 μl significantly saves biochemical reagents.
The study of the hemostasis system is vital in preparing for operations. The main "pain" of the laboratory technician is the effect of lipemia or bilirubinemia on the optical density of the sample. This often leads to false blood clotting indicators.
Modern BioSystems coagulometers use clot registration methods that ignore the turbidity of the sample. This allows obtaining accurate data even in complex patients with cardiovascular diseases without the need for repeated blood sampling.
Analysis of electrolytes (Na+, K+, Cl-) is critical in intensive care. In such situations, the main problem is time: a delay in the result can be fatal. Diestro electrolyte analyzers are designed specifically for conditions where instant accuracy is required.
The automated Diestro Auto Plus model provides high measurement speed (up to 60 samples per hour) with a minimum sample volume of 40 μl. Main advantages:
• Automatic self-diagnosis: the device independently monitors the condition of the electrodes and the consumption of reagents.
• Adaptability: compact dimensions allow installing the analyzer directly in intensive care units.
• Simplicity of the interface: the touch screen and connection to the LIS minimize the time for document flow.
General urinalysis has long depended on the subjective assessment of the laboratory technician. 77 Elektronika has solved this problem by fully automating the process. Semi-automatic devices such as DocUReader 2 Pro eliminate errors associated with the human factor.
For large laboratories, the fastest in the LabUReader Plus 2 line is the ideal solution, processing up to 500 tests per hour. The use of standardized LabStrip U11 Plus test strips guarantees the stability of results and the detection of pathologies at an early stage.
The true efficiency of a medical institution lies in creating a single diagnostic circuit. The use of systems from BioSystems, Diestro and 77 Elektronika simultaneously solves the problem of data fragmentation. When the equipment works in synergy, the laboratory receives a complete clinical picture of the patient's condition.
From a management point of view, European equipment from the supplier Medigran reduces hidden costs. They often arise due to the need for repeated tests or simple equipment. The rational use of reagents and high reliability make such an investment justified in the first year of operation.
Conclusion
The introduction of automated analyzers is the only way to reduce the number of diagnostic errors. BioSystems, Diestro and 77 Elektronika technologies transform routine research into a fast and accurate process, which directly improves the quality of life of patients.

Neurosurgery is one of the most demanding branches of surgery, where even microscopic structures are of critical importance for the outcome of the operation. Visualization of the surgical field directly affects the accuracy of manipulations, patient safety and the efficiency of the doctor's work.
Binocular loupes are an important tool for a neurosurgeon, allowing for increased detail, reduced eye fatigue and improved ergonomics of work. Working with small anatomical structures, vessels and nerve fibers requires stable magnification, high optical quality and ergonomic comfort for the surgeon during long operations.
A common mistake is to immediately choose loupes with high magnification (4x, 6x and more). However, practical experience shows that the transition to high magnifications should be gradual.
Binocular loupes with 2.5x magnification are considered the optimal start, which provide a balance between magnification, field of view and depth of field. This magnification allows you to quickly adapt to working with optics without overloading your vision and cervical spine.
The HR (High Resolution) series of binocular loupes from the leading German manufacturer HEINE Optotechnik uses aspheric lenses that differ from classic spherical shapes. Aspheric lenses have a complex surface geometry that allows you to:
• reduce spherical aberrations,
• provide a clear image (uniform sharpness) across the entire field of view,
• increase the contrast and sharpness of small structures,
• obtain high resolution without distortion at the edges
The 2.5x HR loupes use a prismatic design that allows you to obtain compact optics with a wide field of view and a comfortable working distance.
For magnifications of 3.5x, 4x and 6x, HEINE uses an aspheric optical system of cylindrical shape HRP (High Resolution Prism). Accordingly, the higher the magnification, the smaller the field of view.
The HRP prismatic aspherical optical system provides:
• maximum optical resolution at high magnification,
• stable optical axis,
• reduction of chromatic aberrations,
• minimal optical distortions at high magnification.
HRP 3.5x, 4x, 6x binocular loupes are used in microsurgery, vascular neurosurgery, work with nervous structures and deep operating fields (manipulations with microvessels, neurostimulators, tumor tissues and small brain structures).
Pupillary Distance (PD): a critical parameter for accuracy
Interpupillary distance (PD) is a key parameter when setting up binocular loupes.
Correct PD provides:
• precise alignment of optical axes,
• absence of double images,
• errors in spatial coordination,
• minimal strain on the eyes and brain.
Individual PD adjustment ensures correct convergence of optical axes and accurate depth perception, which is critical for neurosurgery. Incorrectly adjusted PD leads to rapid fatigue, headaches and reduced precision of manipulations.
Illumination of the operating field: LoupeLight2 and ML4 LED
Optics without high-quality illumination do not give the full effect. Therefore, binocular loupes can be placed on illuminators, and mounted on a frame, hoop or helmet.
A compact illuminator, on the frame of which or on the hoop mount binocular loupes are mounted directly. This provides:
• concentrated light in the viewing area,
• minimal shadows,
• synchronization of the optical and light axes.
Professional surgical illuminator with high light intensity and the ability to precisely adjust the beam direction.
LEDHQ technology: natural color reproduction
HEINE uses its own LEDHQ technology (LED in HEINE Quality), which provides:
• natural color reproduction without distortion
• stable color temperature,
• high color rendering index (CRI),
• no change in tissue color over the entire service life.
This is critical for neurosurgery, where the distinction of vessels, nerve structures and tissues depends on color accuracy.
Practical application in neurosurgery
In neurosurgery, binocular loupes are used for:
• microsurgical access to vessels and nerve structures,
• resection of brain and spinal cord tumors,
• vascular anastomoses and neurovascular procedures,
• implantation of neurostimulators and catheters.
Binocular loupes with properly selected magnification and illumination allow:
• to improve visualization of small anatomical structures,
• to increase the accuracy of microsurgical manipulations,
• to reduce the time of surgery, reduce the risk of complications,
• to reduce the strain on the surgeon's eyes and neck,
• to increase ergonomics and productivity.
Conclusion
Binocular loupes are an effective tool for neurosurgery, in particular HEINE binocular loupes, which combine high-precision aspheric optics, high-magnification prismatic systems and professional illumination. A gradual transition from 2.5x to higher magnification, correct adjustment of the interpupillary distance. The use of coaxial lighting ensures maximum diagnostic and surgical accuracy when working with critical microstructures.

Medical equipment is the basis of modern medicine: from diagnostics to interventions, monitoring and ensuring patient safety. In 2026, clinics and medical institutions will implement new technological solutions that significantly increase the effectiveness of treatment, improve the accuracy of diagnostics and ensure the comfort of patients and staff.
Ultrasound diagnostics remains one of the key non-invasive examination methods. Modern ultrasound systems are equipped with automatic measurement modules, in particular, AI tools that reduce the influence of the human factor and provide standardized results. The obtained data is automatically stored in electronic medical records, simplifying dynamic patient monitoring.
In modern ultrasound sensors, in particular in Alpinion systems, a plastic aperture is used as an element of the design of the sensor's working surface. The use of special medical polymers ensures high mechanical strength of the sensor while simultaneously reducing its mass, which increases the convenience of the doctor's work during long examinations. The plastic aperture is characterized by resistance to repeated disinfection and chemical influences. At the same time, the design of the plastic lens ensures uniform transmission of ultrasound waves into the tissue, minimizing unwanted reflections at the contact interface. This improves the quality of the obtained image, which is especially important when examining surface structures, vessels and working in Doppler modes.
X-ray diagnostics remains one of the key imaging methods in clinical practice due to the combination of informativeness, speed and accessibility. In 2026, the main development of X-ray equipment is aimed at the complete digitalization of the image acquisition process, optimization of the dose of ionizing radiation and integration of devices into a single information infrastructure of a medical institution.
Modern X-ray systems are equipped with flat-panel digital detectors, which provide high spatial resolution and stable image quality at reduced radiation doses, and X-rays are also equipped with high-frequency generators, X-ray tubes with increased heat capacity and active cooling, which ensures stable operation even under high load. Built-in dosimetric modules automatically record the actual dose during each examination, and the data is stored in electronic medical records for individual dose control.
Medical monitors play a key role in displaying X-ray, endoscopic, ultrasound and intraoperative images.
Unlike conventional monitors, the key characteristic of medical monitors is high resolution and stable brightness, which is why modern medical monitors are equipped with front sensors that continuously monitor the brightness level and transmit data to the automatic stabilization system. In case of deviations, the system corrects the light flux, maintaining constant image quality. The brightness of such monitors is calibrated according to the DICOM standard, which ensures accurate transmission of grayscale in diagnostic studies. Conventional monitors do not have similar control mechanisms, so their brightness quickly decreases - up to 30% in the first year and up to 50% in the second, which can negatively affect the accuracy of image interpretation.
Modern ventilators provide a wide range of ventilation modes, from volume- and pressure-controlled to spontaneous patient support. Ventilator algorithms adapt oxygen delivery and inspiratory volume to changes in lung mechanics, patient weight, and clinical status, improving ventilation efficiency and reducing the risk of barotrauma. In addition, modern systems support patients with partial spontaneous ventilation, synchronizing with their own breathing and reducing discomfort and the risk of barotrauma.
In 2026, ventilators will be equipped with integrated monitoring systems for key parameters: inspiratory and expiratory volume, respiratory rate, airway pressure, oxygen-to-carbon dioxide ratio, and minute ventilation. These data are displayed on the patient monitor in real time and stored in the electronic medical record for dynamic analysis. Multi-level alarm systems signal critical changes in ventilation parameters, gas leakage, tube obstruction, or device shutdown. This allows medical personnel to respond quickly to potentially dangerous situations.
Electrocardiography remains the basic method of functional diagnostics in cardiology and emergency medicine. In 2026, electrocardiographs will be equipped with digital analysis algorithms that allow automatic calculation of key parameters - PR, QRS, QT intervals, heart rate, and the electrical axis of the heart.
Modern 3-, 6-, and 12-channel ECG systems provide high accuracy of signal registration due to effective interference filtering and stable operation even in difficult clinical conditions. Digital algorithms form the basis of intermediate interpretative conclusion, which reduces analysis time. The data is stored in the internal memory or transmitted to the electronic system for further comparison of results in dynamics.
Modern patient monitors provide simultaneous measurement and display of a wide range of physiological parameters, including electrocardiogram (ECG), heart rate, blood oxygen saturation (SpO₂), non-invasive and invasive blood pressure, respiratory rate, body temperature, as well as gas exchange indicators.
Thanks to advanced filtering algorithms and highly sensitive sensors, stable signals are provided even with patient mobility or electromagnetic interference. The monitors are also equipped with multi-level alarm signals that respond to parameters exceeding the normal range and help staff quickly assess the criticality of the situation.
In 2026, patient monitors are actively integrated with central monitoring stations, which allow monitoring the condition of several patients simultaneously.
Endoscopic equipment is one of the key components of modern diagnostics and treatment, as it allows visualization of internal organs and cavities without the need for open surgical intervention. In 2026, the development of endoscopic systems is aimed at improving image quality, ergonomics of the doctor's work and patient safety.
In 2026, significant attention is paid to the optical characteristics of endoscopes. The use of multi-lens systems and improved light-conducting materials allows for uniform illumination of the field of view without darkening zones. High image clarity and contrast contribute to the early detection of pathological changes, including inflammatory processes, neoplasms and structural anomalies. An important aspect is the stability of color rendering, which allows the doctor to correctly assess the condition of tissues and vessels, as well as distinguish normal anatomical structures from pathological ones.
Medical furniture is an integral part of the medical and diagnostic environment and directly affects patient safety, ergonomics of medical staff work and the effectiveness of clinical procedures. In 2026, the development of medical furniture is aimed at combining mechanical reliability, precision adjustments and compatibility with high-tech medical equipment.
Operating tables in 2026 are characterized by a multi-section design and a wide range of adjustments for the patient's body position. Electromechanical and electrohydraulic systems allow for precise adjustment of the height, tilt and position of the sections, which is critical for ensuring optimal access to the operating field. Modern operating tables are compatible with X-ray and C-arm systems, which allows intraoperative control without moving the patient. The stability of the structure and the high permissible load mass ensure the safety of patients during long surgical interventions.
New generation gynecological chairs are developed taking into account the anatomical features of patients and the needs of the doctor. Electric drives provide smooth adjustment of the backrest, seat and footrests, which allows you to quickly switch between different examination or treatment modes. Disinfection-resistant materials and a well-thought-out design contribute to compliance with sanitary and hygienic requirements and reduce the risk of cross-infection.
Modern operating lights use multi-segment LED modules that form uniform shadowless illumination of the operating field. Even with partial overlap of the light flux, the illumination remains sufficient, which is important during complex interventions. The high color rendering index (CRI) of modern lamps allows you to accurately distinguish shades of tissues, vessels and blood, which directly affects the quality of clinical decision-making during surgery.
In 2026, operating lights are equipped with flexible control systems, including remote settings via a mobile application, which allows you to change the intensity and color temperature without physical contact with the equipment. This helps to maintain the sterility of the operating field and quickly adapt the lighting to the needs of the intervention. Considerable attention is also paid to integration with cameras and video recording systems of operations, which allows not only to document interventions, but also to use materials for training and interdisciplinary consultations.
In 2026, medical equipment forms a single digital environment of the clinic, where diagnostic and monitoring systems work synchronously. The key remains the accuracy of measurements, the stability of technical parameters, the automation of analysis and integration with electronic medical systems. It is this technological consistency that allows to increase patient safety, reduce the risk of errors and ensure a consistently high level of medical care.